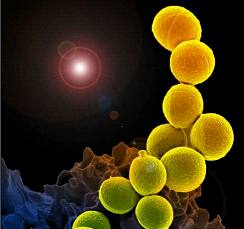
J Intern Med:减少心血管事件,金黄色葡萄球菌是如何做到的?
2016-09-28 Moon 译 MedSci原创
金黄色葡萄球菌细胞壁成分能够诱导免疫细胞产生IL-10,这种细胞因子具有抗动脉粥样硬化作用。因此,在本研究中,我们调查了热灭活金黄色葡萄球菌(HK-SA)能否抑制动脉粥样硬化的发展。 研究纳入了易患动脉粥样硬化的低密度脂蛋白 受体缺乏的小鼠,每周腹腔注射HK-SA两次,喂食西方饮食六周。 结果显示,HK-SA导致腹膜巨噬细胞和脾细胞的IL-10的产量增加1.6倍,血清IL-10的产量增
金黄色葡萄球菌细胞壁成分能够诱导免疫细胞产生IL-10,这种细胞因子具有抗动脉粥样硬化作用。因此,在本研究中,我们调查了热灭活金黄色葡萄球菌(HK-SA)能否抑制动脉粥样硬化的发展。
研究纳入了易患动脉粥样硬化的低密度脂蛋白受体缺乏的小鼠,每周腹腔注射HK-SA两次,喂食西方饮食六周。
结果显示,HK-SA导致腹膜巨噬细胞和脾细胞的IL-10的产量增加1.6倍,血清IL-10的产量增加12倍。此外,主动脉斑块ICAM-1、VCAM-1和CCL2的表达水平显著下降,平均下降40%。HK-SA治疗的小鼠,其炎症Ly-6Chi单核细胞数量减少,循环和脾脏中的Th1和Th17细胞也减少了。募集减毒白细胞显著抑制了动脉粥样硬化斑块处的巨噬细胞和T细胞浸润,最终导致动脉粥样硬化的进展减慢34%。
为了确定腹腔HK-SA的治疗效果,我们在体外使用HK-SA刺激巨噬细胞。结果显示,Toll样受体2(TLR2)在IL-10、Arginase-1、iNOS、TNF-α, PD-L1、CCL22和吲哚胺2,3-双加氧酶表达中的显著增加。研究发现,磷脂酰肌醇3激酶是平衡促炎和抗炎基因表达平衡的关键因子。HK-SA诱导巨噬细胞类似于M2b调节巨噬细胞。
研究表明,HK-SA治疗可诱导巨噬细胞强烈的抗炎反应,产生更多的IL-10,这种反应很大程度上依赖于TLR2和PI3K,且有助于防止动脉粥样硬化的发展。因此,共生的金黄色葡萄球菌可以减少心血管事件。
原始出处:
V. Frodermann,et al.Heat-killed Staphylococcus aureus reduces atherosclerosis by inducing anti-inflammatory macrophages.J Intern Med.Volume 279, Issue 6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管事件#
60
#金黄色葡萄球菌#
67
#葡萄球菌#
58
#Med#
75
继续关注
82
继续学习
89