解读Cell:肠道细菌与病毒的作用,揭示小儿腹泻主要病原体“轮状病毒” 潜在的防治新方法
2019-10-13 佚名 BioArt
相比于细菌,人类对于病毒感染治疗防御措施少之又少,对于病毒感染类似于抗生素的有效治疗方法还没有被发现。细菌通常被认为对压抑病毒感染没有关系。但特定的病毒,比如噬菌体可以侵蚀细菌细胞。在机体被侵蚀的过程中,如果不孕育出抵抗机制,在漫长的进化过程中违背常理,或会被自然选择排除,但我们对于细菌是如何抵抗病毒感染研究有限。
轮状病毒(Rotavirus,RV)是一种非包膜的双链RNA(dsRNA)病毒,仍然是全球范围的主要病害,每年导致数十万儿童出现危及生命的腹泻,也是导致小儿及新生儿腹泻的最主要病原体。RV 从口进入人体,主要感染肠胃上皮细胞,这些细胞存在于一个统称为肠道微生物群的大型生态系统中。肠道微生物群可预防致病菌。例如,抗生素处理的宿主极易被细菌病原体侵殖和患病。这种侵殖阻力被认为反映了特定细菌家族防止特定类别的病原体的能力。然而,微生物群对肠道病毒感染的影响程度并不很清楚。
2019年10月10日,佐治亚州立大学Andrew T. Gewirtz教授团队(一作为石振达博士)在Cell杂志上以长文形式发表了文章Segmented Filamentous Bacteria Prevent and Cure Rotavirus Infection,研究了肠道细菌微生物对轮状病毒感染的影响。
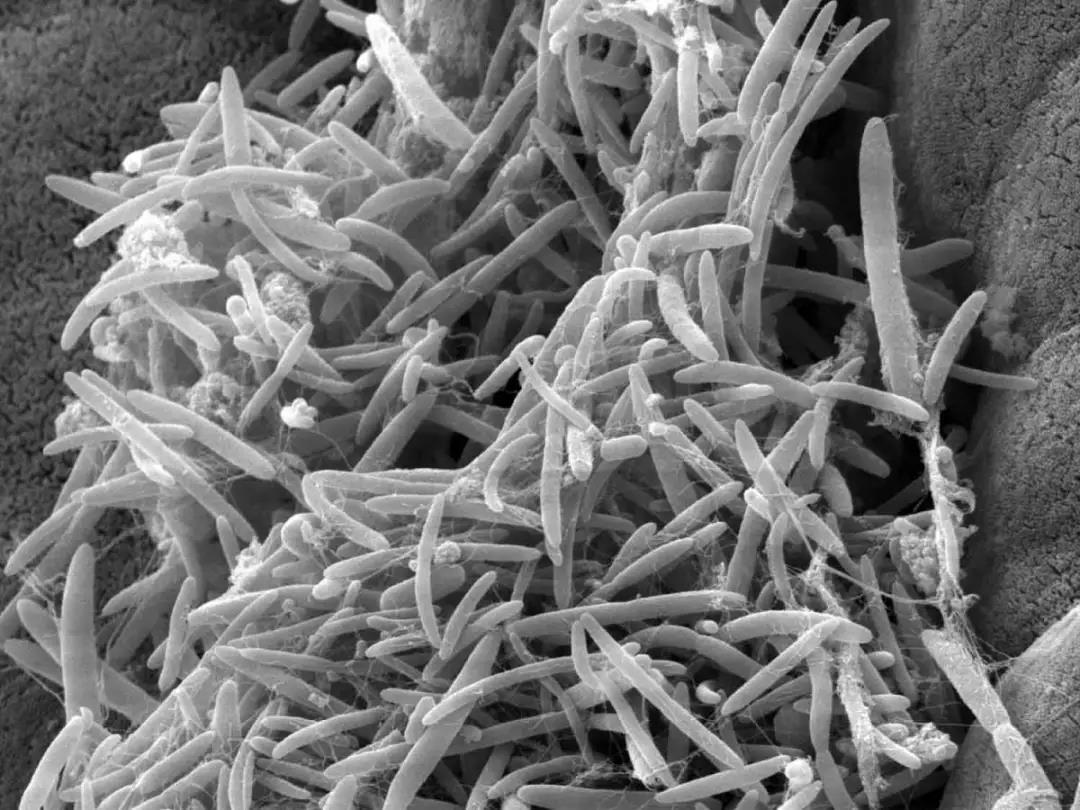
Rag1-knockout(KO)小鼠,与患有严重免疫缺陷的人类一样,它们一旦被RV感染,就会发展为慢性RV感染。在将Rag1-KO小鼠用于研究时,我们无意间发现了一株对RV感染具有高度抵抗力的Rag1-KO小鼠。我们猜想这些小鼠获得了特定微生物群,这赋予了宿主RV的抗性。我们发现它们的RV抗性与固有淋巴细胞(ILC)无关,也不需要干扰素(IFN),它们对于控制大多数病毒至关重要。相反,这些小鼠对RV抗性是由分段丝状细菌(segmented filamentous bacteria,SFB)介导的,这种细菌在防止或治愈RV感染的方向上改变了RV和宿主回肠,这暗示一种新的机制,通过这种机制,肠道微生物群可以改善健康。事实上,我们发现通过对富含SFB的肠道微生物群的移植,接受移植的小鼠达到了“百毒不侵”的状态,对多种肠道病毒和细菌产生了抗性。
结 果
1. 可传播的微生物保护免疫缺陷和有免疫能力的小鼠免受轮状病毒感染
我们将RV-易感Rag1-KO小鼠称为"JAX-RAG",将上述抗RV的Rag1-KO小鼠称为"GSU-RAG"。将JAX-RAG和GSU-RAG小鼠放在同一笼子或从GSU-RAG中移植出肠道微生物群,导致JAX-RAG小鼠获得RV耐性。移植GSU-RAG肠道微生物到无菌(Germ free,GF) Rag1-KO小鼠中产生了对RV完全抗性,而接受JAX-RAG微生物群的GF Rag1-KO小鼠发展为慢性RV感染,说明移植的肠道菌群可以完全保护宿主,而并不需要宿主本身的菌群做出贡献。此外,对具有慢性RV感染的JAX-RAG小鼠进行GSU-RAG肠道微生物群(而不是JAX-RAG的)移植,导致RV抗原释放停止,表明慢性RV感染的治愈。哺乳期RAG幼崽与RV的感染导致水性腹泻。RV 引起的腹泻几乎被 GSU-RAG 消除,但JAX-RAG 粪便不能做到。更多的是,免疫染色和PCR对回肠内RV基因组的定量证实没有RV感染。
类似地,移植GSU-RAG肠道微生物到具有完善免疫系统的野生(WT)小鼠,使宿主获得了对RV的抗性。在成年WT小鼠上,这种保护性与移植后RV感染的早晚有关。在移植GSU-RAG肠道微生物后两日内对其进行RV感染,宿主会被完全保护,不会被感染;然而7日后进行感染,宿主只会被部分保护。在幼年WT小鼠(1周和3周)上,进行移植和RV感染,完全的RV保护性会产生,比如水样腹泻几乎会被完全消失。
2. 探寻保护机制以及起关键抗病毒的微生物
我们尝试了中和移植可能导致宿主产生的抗病毒因子,比如IL-22,IFN-,但抗病毒作用并未消失。我们还尝试了探寻其他肠道免疫细胞对这个抗病毒现象的贡献,通过运用固有淋巴细胞缺失的小鼠,以及探寻免疫细胞的数量变化,并且进行移植肠道免疫细胞,但这些实验都表明,这些免疫因子和免疫细胞对于这个RV抗性的表现性贡献有限,因此这种抗RV 感染的机制有别于常见抗病毒的机制。
固有淋巴细胞缺失(ILC)的小鼠,这株小鼠没有T细胞、B细胞和NK细胞;粒细胞、巨噬细胞和突出细胞数量都有明显减少。这样在这株小鼠宿主体内剩余的免疫细胞,以及抗病毒的机制已经很有限了。我们研究了GSU-RAG微生物是否有能力在体外降低RV感染能力。结果令人振奋,从粪便中过滤出的肠道菌群可以在没有免疫细胞的条件下减少RV感染,并且这种抗病毒作用不仅局限于RV,但延伸到其他病毒,包括VSV,IAV,和reo病毒都被不同程度的,在体内和体外,减少了毒力。
对肠道菌群进行体外混合抗生素处理,而不是混合抗真菌处理,这种抗RV的保护作用随之消失,证明关键抗病毒微生物对抗生素敏感。随后更具体的抗生素处理表明,关键抗病毒的微生物对卡那霉素耐受。通过对具有RV抵抗性的微生物群加热、过滤和抗生素的处理,然后稀释并移植到无细菌小鼠,最后进行微生物群落分析。这种方法表明,一株新的分段丝状细菌(SFB)存在于被移植并且产生RV抵抗性的小鼠肠道内。这株SFB占被移植小鼠肠道细菌总量超过95%,并且它足以使小鼠对RV感染和相关腹泻产生抗性。通过基因测序,RV感染测试,肠道切片染色,移植GSU-RAG混合肠道菌群和这株SFB可以造成相似的宿主表型,包括肠道上皮细胞增生,肠道基因表达的改变。这种肠上皮增生现在被认为和抗肠道病原微生物感染有密切关系。
总 结
轮状病毒与多种微生物群共生在肠道上皮细胞,从而打开微生物影响 RV感染的可能。虽然清除RV通常需要适应性免疫,但我们无意间发现了抗RV免疫缺陷的小鼠,而通常来说清除病毒感染紧紧依赖于免疫系统,而免疫缺陷的宿主难于清除病毒感染,从而被病毒慢性感染,乃至终生被感染。我们假设,这种RV抗性反映了抵抗RV感染的微生物的存在。具体的是,这种RV抵抗性可通过共宿和粪便移植来传播。这种保护作用与先前定义的RV阻抗因素无关,包括固有免疫细胞ILCs,干扰素、IL-17和IL-22。SFB在回肠的定植诱导宿主基因表达的变化,并加速上皮细胞周转。含有SFB的粪便与RV共同孵育,降低了RV体外感染率,揭示了直接中和RV作用的可能。因此,独立于免疫细胞,SFB提供保护某些肠道病毒感染和相关腹泻病。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#主要病原体#
63
#CEL#
68
#Cell#
67
#新方法#
76
#肠道细菌#
93
#轮状病毒#
75
#病原体#
74