铜绿假单胞菌:发病机制、毒力因子、抗生素耐药性、与宿主的相互作用、技术进展和新疗法
2022-06-29 小文子 MedSci原创
研究对铜绿假单胞菌生物性状、毒力因子、侵袭性调节因子和宿主对其感染的防御模式等方面的进展进行了全面综述和讨论,指出了未来研究的新方向。
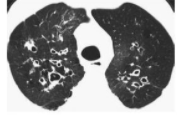
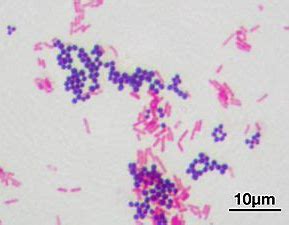
铜绿假单胞菌(P. aeruginosa)是一种革兰氏阴性机会致病菌,可感染囊性纤维化、烧伤、免疫缺陷、慢性阻塞性肺疾病、癌症和需要机械通气的重度感染患者。Signal Transduction and Targeted Therapy杂志综述了铜绿假单胞菌在毒力因子、基因表达调节因子、分泌系统、群体感应和抗生素耐药性的调节和功能机制,以及宿主-病原体相互作用、新技术和治疗等方面的研究进展。
铜绿假单胞菌能够通过分泌多种毒力因子来适应宿主体内的不利环境,从而使宿主成功感染并致病,如脂多糖、外膜蛋白、鞭毛、菌毛和其他黏附素、6型分泌系统等。所有这些毒力因子的调控都依赖于细胞密度,通过释放关键群体感应(QS)的自动诱导物(如Las、Rhl、Pqs和Iqs)。关键群体感应可能通过分层信号模式帮助适应恶劣的宿主环境并茁壮成长,导致囊性纤维化患者持续感染,即使在药物、医疗环境和生活条件大幅改善的情况下,仍无法完全治愈。因此,关键群体感应系统以及其他一些关键毒力因子,如六种类型的分泌系统、双组分系统,已经成为理解这种细菌机理的关键因素。
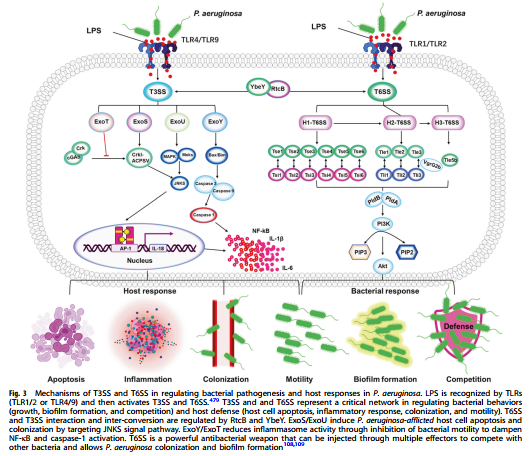
铜绿假单胞菌几乎存在于任何地方和任何环境条件下。免疫抑制人群对铜绿假单胞菌极度敏感。作为宿主防御系统的第一道防线,先天性免疫系统通过多种机制,如吞噬作用和炎症反应,在与铜绿假单胞菌的斗争中起着至关重要的作用。几种类型的宿主系统,如模式识别受体、质膜信号、细胞内酶和分泌细胞因子/趋化因子参与了针对细菌感染的炎症反应。尽管抑制铜绿假单胞菌侵袭需要良好平衡的炎症反应,但过度活跃的炎症与疾病快速进展、组织损伤甚至死亡相关。一些宿主分子包括胞质蛋白膜联蛋白A2(AnxA2)、自噬相关蛋白7(ATG7)、NLRC4以及非编码RNA(lncRNA和microRNA),也与铜绿假单胞菌诱导的炎症和/或宿主防御机制的其他方面有关。
此外,许多技术进展,如生物信息学、代谢组学、scRNA-seq、纳米颗粒、药物筛选和噬菌体治疗,已被用于提高对铜绿假单胞菌发病机制和宿主防御的理解。然而,铜绿假单胞菌与宿主免疫应答之间的相互作用仍有许多有待发现,包括已知或未注释的细菌毒力因子的耐药机制以及哺乳动物细胞信号通路。
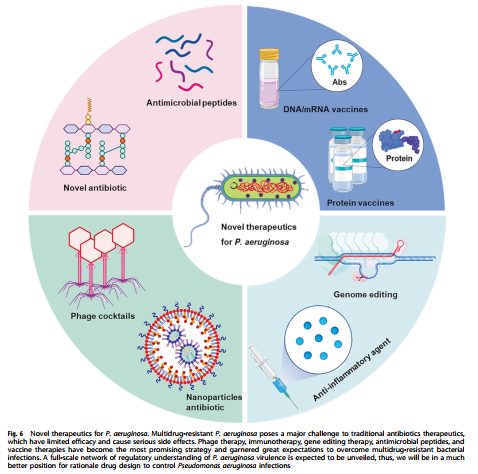
抗生素的广泛使用和有效抗菌剂的开发带来巨大挑战,需要新的理论和实践平台来筛选和开发新型药物治疗难治性感染,尤其是多重耐药菌株引起的感染。受益于研究工具和技术的进步,解析这种病原体的特征已经进入分子和机制细节以及动态和整体的观点。研究对铜绿假单胞菌生物性状、毒力因子、侵袭性调节因子和宿主对其感染的防御模式等方面的进展进行了全面综述和讨论,指出了未来研究的新方向。
原文出处:
Qin, S., Xiao, W., Zhou, C. et al. Pseudomonas aeruginosa: pathogenesis, virulence factors, antibiotic resistance, interaction with host, technology advances and emerging therapeutics. Sig Transduct Target Ther 7, 199 (2022). https://doi.org/10.1038/s41392-022-01056-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#相互作用#
112
#宿主#
125
#抗生素耐药#
101
#互作#
111
#新疗法#
110
#抗生素耐药性#
101
学习了,谢谢分享
96