Br J Anaesth:脑电图抑制持续时间不能预测志愿者全身麻醉恢复时间及认知障碍程度
2020-01-28 anesthGH “罂粟花”罂粟花
昏迷和全身麻醉时,脑电图波会出现爆发抑制。据推测爆发抑制是一种较难恢复的深麻醉状态,然而并没有直接证明。本研究探讨脑电图爆发抑制与志愿者麻醉后意识恢复的关系。
背景与目的
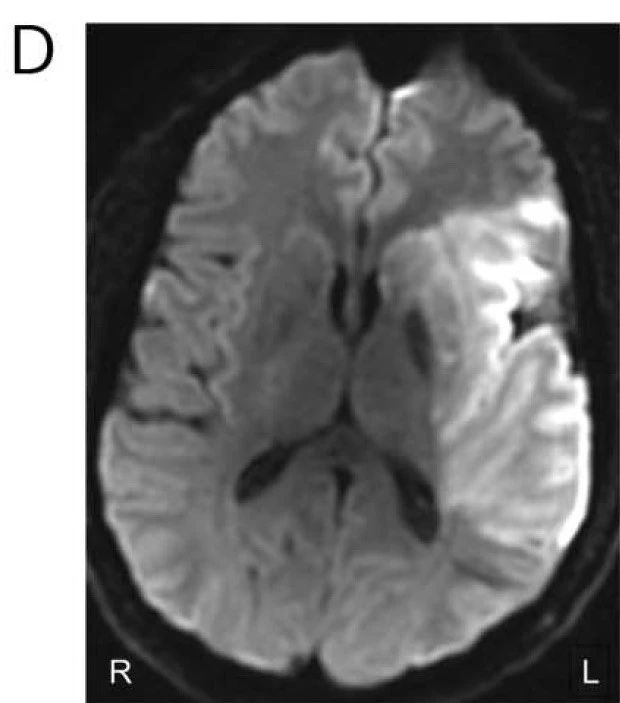
昏迷和全身麻醉时,脑电图波会出现爆发抑制。据推测爆发抑制是一种较难恢复的深麻醉状态,然而并没有直接证明。本研究探讨脑电图爆发抑制与志愿者麻醉后意识恢复的关系。
方 法
本研究纳入了27名健康志愿者(9名女性/18名男性),用1.3 MAC异氟醚麻醉3小时,麻醉期间记录脑电图。利用频谱成分分析法计算脑电图抑制和非抑制的持续时间。参与者完成了数字符号替换测试和精神运动警惕测试试验。
结 果
受试者表现出受抑制脑电图多种特征的显着变异性。为了验证上述假设,对于个体,为提高将脑电图抑制特征与预测恢复时间的关系而构建了两种精确模型:一种包含抑制相关特征,另一种不包含抑制相关特征。与我们的假设相反,增加脑电图爆发抑制相关特征并不能提高模型预测恢复时间的能力。此外,与麻醉前相比,脑电图爆发抑制量和认知功能下降没有相关性。
结 论
脑电波爆发抑制并不是健康成人麻醉后恢复时间或认知障碍程度的决定因素。
原始出处:
Shortal BP, Hickman LB, Mak-McCully RA,etal. Duration of EEG suppression does not predict recovery time or degree of cognitive impairment after general anaesthesia in human volunteers. Br J Anaesth. 2019 Jun 12. PMID: 31202561.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#志愿者#
105
#ANA#
67
#EST#
86
学习了
132
#持续时间#
72