DCR:改变生活方式可以降低结直肠癌择期手术患者术后并发症的发生率
2021-06-30 MedSci原创 MedSci原创
运动已经被广泛地证明可以维持和恢复机体、组织、细胞和分子水平的内稳态,以预防或抑制多种疾病如肿瘤、心脏病、高血压、糖尿病等。
运动已经被广泛地证明可以维持和恢复机体、组织、细胞和分子水平的内稳态,以预防或抑制多种疾病如肿瘤、心脏病、高血压、糖尿病等。而术前运动疗法(Pre-operative exercise therapy)也被报道可以有效缩短病人术后恢复及住院时间,其中一个主要的机制是运动可以系统的提高患者术前的心血管储备能力,从而提高全身应对系统性失调的耐受。研究表明,患者术前生活方式与术后并发症之间可能存在关联。因此,本项研究旨在评估术前生活方式与接受结肠直肠癌择期手术的患者术后并发症之间的关联。

研究人员将诊断为结直肠癌择期手术的患者进行基线的临床资料收集,使用问卷收集有关吸烟习惯、饮酒量、BMI 和身体活动的数据。术后并发症的发生情况通过病例系统进行收集。多变量逻辑回归模型用于确定哪些术前生活方式因素与术后并发症相关。
研究结果发现结直肠癌择期手术的患者的术后并发症发生率为 28.5%,并发症的出现会导致住院时间大幅延长(12 天 vs. 5 天,p<0.001)。与较高的术后并发症发生率独立相关的危险因素是 ASA 分类 II(OR 1.46;95% CI 1.05-2.04,p=0.03)和 III-IV(OR 3.17;95% CI 1.96-5.12,p<0.001)、吸烟状况(OR 1.62;95% CI 1.02-2.56,p=0.04)和直肠肿瘤(OR 1.81;95% CI 1.28-2.55,p=0.001)。而BMI、饮酒和体力活动与术后并发症无关。然而,在对 200 名 ASA III-IV 患者的亚组分析中,术前高体力活动与较少的术后并发症相关(OR 0.17;95% CI 0.03-0.87,p=0.04)。
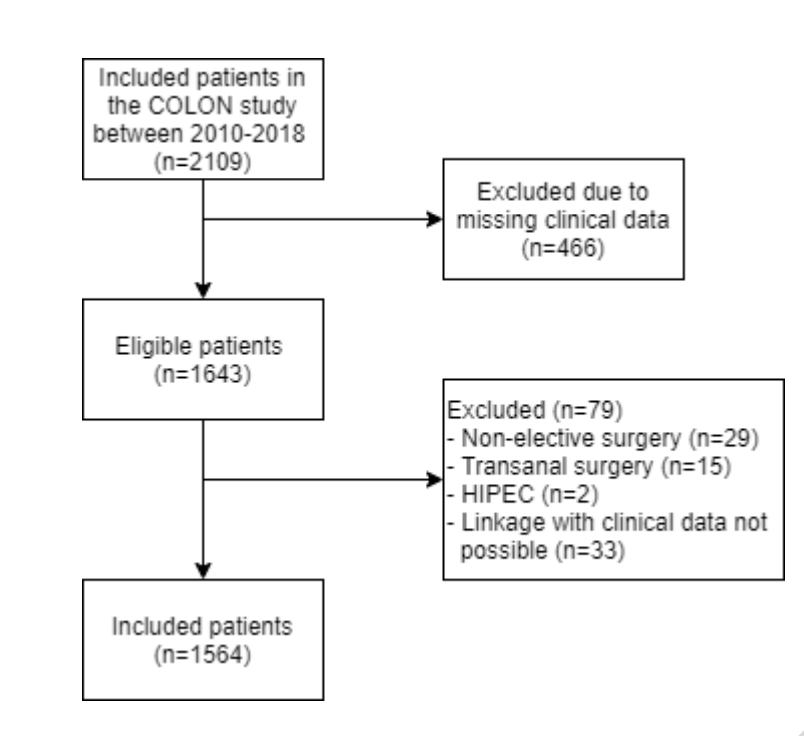
图:患者筛选流程图
本项研究证实改变生活方式,如减少吸烟和增加身体活动,可以降低结直肠癌手术后的术后并发症。在整个研究人群中,目前吸烟与术后并发症风险增加有关,而术前高体力活动仅与ASA III-IV 患者术后并发症风险降低有关。
原始出处:
Loogman, Lisanne. Et al. The Association Between Modifiable Lifestyle Factors and Postoperative Complications of Elective Surgery in Colorectal Cancer Patients. Diseases of the Colon & Rectum.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#并发#
81
#发生率#
112
#择期手术#
82
#结直肠#
95
受益匪浅
103
学习了
81