Eur Radiol: 肾脏CT不同期相对肾肿块纹理分析的有何影响及意义?
2021-03-15 shaosai MedSci原创
现阶段,运用纹理分析(TA)对肾脏肿块进行评价的方法已在多项研究中被使用且证明有效。

现阶段,运用纹理分析(TA)对肾脏肿块进行评价的方法已在多项研究中被使用且证明有效。应用计算机断层扫描(CT)和磁共振成像(MRI)评价的肾脏肿块的一阶和二阶TA可用于诊断肾脏良性肿瘤(如乏脂血管平滑肌脂肪瘤[fp-AML]和嗜酸细胞瘤[6])、肾细胞癌(RCC)亚型及RCC分级。
肾脏CT扫描方案包括平扫(NECT)期、皮髓质(CM)期、肾造影(NG)期。目前尚不清楚CT增强期是否影响肾脏肿块的TA,对于哪个增强期应优先使用尚无共识。
近日,发表在European Radiology杂志的一项研究比较了肾脏CT扫描方案中,平扫(NECT)期、皮髓质(CM)期、肾造影(NG)期上的肾实性肿块的纹理分析(TA)特征的差异及诊断性能,明确了应使用哪一期相作为诊断的最佳期相。
本研究共纳入177例肾实性肿块(116例肾细胞癌:透明细胞癌51例,乳头状细胞癌40例,嫌色细胞癌25例。良性肿瘤61例:49例嗜酸细胞瘤,12例脂肪含量低的血管平滑肌脂肪瘤),每位患者均在2012年至2017年期间行三期CT扫描。两名放射科医生使用盲法独立评估了肿瘤的异质性(5点Likert量表)并对肿瘤进行分期。比较了组间、期像间的TA特征(N = 25)。比较了RCC与良性肿瘤及cc-RCC与其他肿块的准确性(曲线下面积[AUC])。
主观上,不同期相之间肿瘤的异质性(p <0.01)及同一期像内肿瘤之间的异质性差异显著(p = 0.03 [NECT]和p <0.01 [CM,NG])。观察者间的一致性为中度到显著(组内相关系数= 0.55-0.73)。
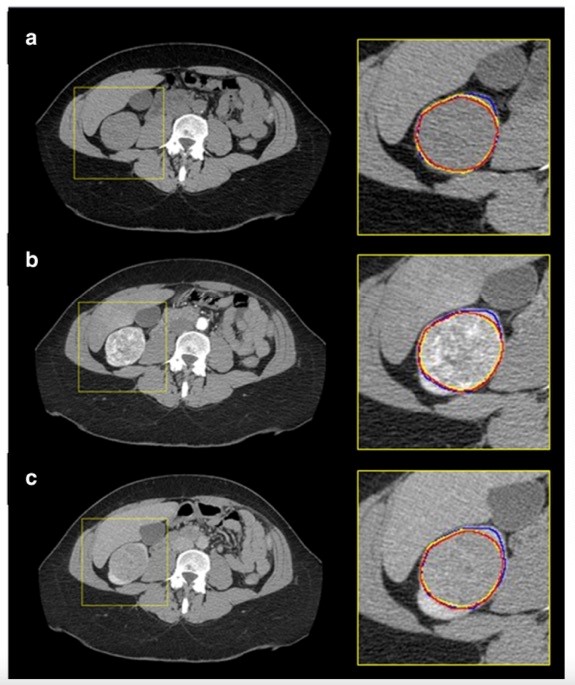
图1 52岁女性右肾下极透明细胞肾细胞癌,(a)平扫CT (NECT)、(b)皮髓质(CM)期和(c)肾造影(NG)期。用黄色表示放射科医师1,第一轮;红色代表放射科医师1第二轮;蓝色代表放射科医生2。在这项研究中,分割在放射科医师内部及之间的再现性极好。
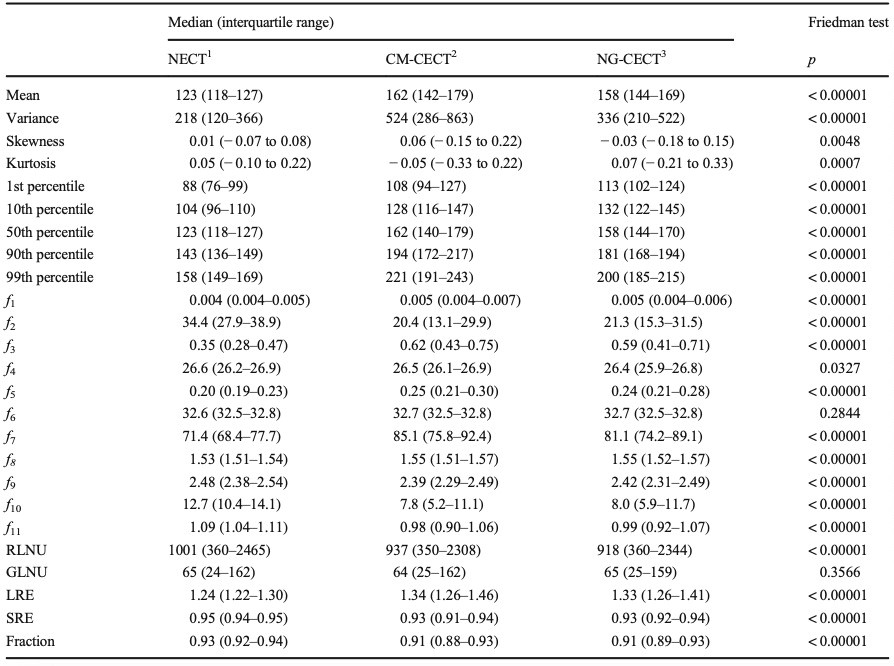
表1 评估肾脏肿块CT方案三期纹理特征之间差异的Friedman测试。除GLNU和f6外,TA各期间差异为92.0%(23/25),差异有统计学意义(p < 0.05)。

表2 定量纹理特征在肾细胞癌与良性肾肿块诊断中的应用。RCC与良性肿瘤相比,纹理特征的AUC与CM和NG的差异无统计学意义(p > 0.05),但在纹理特征的AUC中,CM和NG比NECT高20%(5/25)和28% (7/25)(p < 0.05)。

表3 定量纹理特征诊断cc-RCC与其他肾肿块的ROC分析。cc-RCC与其他肿块相比,36%(9/25)和40% (10/25)CM期图像的AUC高于NECT和NG期图像(p < 0.05)。
在不同CT增强期像主观和定量评价肾肿块时,其纹理分析的结果有所不同。在比较肿块和区分cc-RCC与其他肿块时,皮髓质期具有最高的鉴别诊断价值。当将使用不同CT扫描方案的患的数据结合起来进行研究时,应更仔细地分析用于肾脏肿块诊断、分级和分期的纹理分析特征的差异,因为这些差异不仅与所研究的肿瘤本身有关,也与CT不同期相有关。
原始出处:
Kathleen Nguyen,Nicola Schieda,Nick James,et al. Effect of phase of enhancement on texture analysis in renal masses evaluated with non-contrast-enhanced, corticomedullary, and nephrographic phase-enhanced CT images.DOI:10.1007/s00330-020-07233-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











可以学习了
67
#同期#
107
#纹理分析#
71
#肿块#
65
我需要积分
107