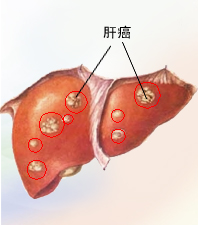
JAMA Oncol: 个体化自适应立体定向放疗治疗肝癌 结果超预期
2017-08-14 呆毛 肿瘤资讯
先前存在肝功能异常的患者在肝肿瘤个体化治疗中获益最大,可以最大限度地控制肿瘤和减少肝衰竭的风险。该试验中研究者设计了一项个体化的适应性试验来检验这一假设,即根据肝功能的变化来优化每个患者的治疗参数。研究结果优于预设效果,提示个体化适性放疗策略可能代表一种新的治疗模式,其剂量基于个体,而非基于整个人群,可使患者更容易耐受治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#自适应#
89
#Oncol#
74
#立体定向#
70
#定向#
74
#个体化#
77
#立体定向放疗#
95