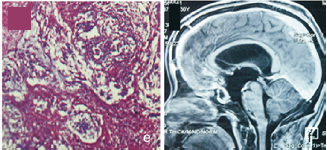
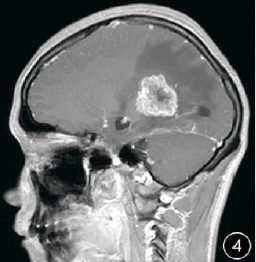
成人不典型鞍区毛细胞型星形细胞瘤1例
2019-10-11 谢民 武志 雒以诚 丁涛 国际神经病学神经外科学杂志
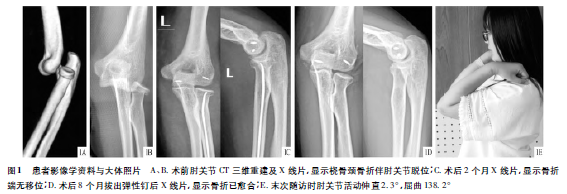
患者男,30岁。因“视力进行性下降1年,行走不稳半年”于2017年12月1日入院。眼科检查:右眼视力0.08,左眼指数20CM,眼底视乳头水肿,边界消失,视野检查无法配合完成;双侧轮替、指鼻及跟膝胫试验欠稳准,余无阳性体征。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#毛细胞型#
60
#不典型#
66
#细胞瘤#
55
#鞍区#
0