Ann Surg.:PET与CT均不宜预测放化疗前后直肠癌患者缓解情况
2013-05-06 ecoliDH5 网络
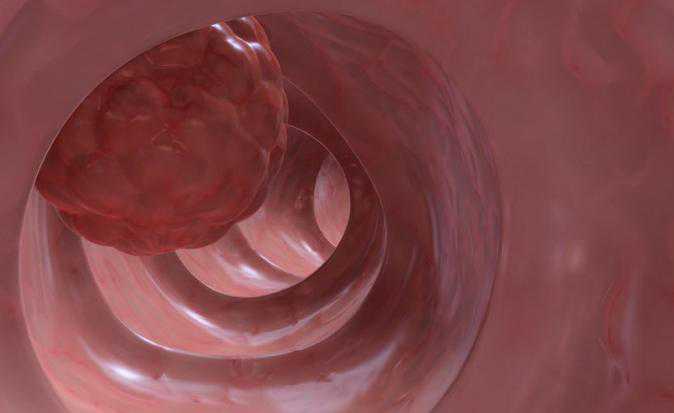
直肠癌患者在放化疗后,进行非手术治疗的一个主要干扰就是,无法对术前病理完全缓解进行判定。因此,美国纽约纪念斯隆-凯特琳癌症中心Jose G. Guillem博士等人进行了一项前瞻性研究,在判定经放化疗治疗的直肠癌病理完全缓解(pCR)方面,前瞻性地对氟脱氧葡萄糖正电子放射断层成像技术(FDG-PET)以及计算机断层成像技术(CT)进行对比。这项研究结果于2012年11月26日在线出版的《外科年鉴》
直肠癌患者在放化疗后,进行非手术治疗的一个主要干扰就是,无法对术前病理完全缓解进行判定。因此,美国纽约纪念斯隆-凯特琳癌症中心Jose G. Guillem博士等人进行了一项前瞻性研究,在判定经放化疗治疗的直肠癌病理完全缓解(pCR)方面,前瞻性地对氟脱氧葡萄糖正电子放射断层成像技术(FDG-PET)以及计算机断层成像技术(CT)进行对比。这项研究结果于2012年11月26日在线出版的《外科年鉴》(Annals of Surgery)杂志上得到发表。
该项前瞻性研究共招募了121例直肠癌患者。研究人员在新辅助放化疗前后,对患者进行FDG-PET扫描以及螺旋CT扫描。并通过对PET以及CT扫描结果的共识性解读,对病情的确定性进行分类(5分评定量表)。通过受试者工作特征曲线(AUC)线下面积,估算出PET扫描和CT扫描对病理完全缓解(ypT0)与不完全缓解(ypT1-4)能鉴别力的准确性。
研究发现,在参试的121例患者中,21例(21%)患者出现病理完全缓解。在鉴别病理完全缓解与不完全缓解准确性方面,PET扫描和CT扫描均同样不完全 (二者AUC = 0.64, P= 0.97)。在这26例病理完全缓解的患者中,通过PET扫描和CT扫描方法,分别有14例(54%)患者和5例患者(19%)被认定为完全缓解。在95例病理不完全缓解的患者中,通过PET扫描和CT扫描方法,则分别有63例(66%)患者和90例患者(95%)被认定为不完全缓解。研究人员认为,PET各单项参数,包括视觉响应值、平均标准吸收值(SUVmean)、最大SUV(SUVmax)以及病变糖酵解总量,均不能准确地对病理完全缓解进行识别(AUC = 0.57-0.73)。
Jose G.Guillem博士等人据此认为,在识别病理完全缓解与不完全缓解方面,PET扫描和CT扫描均无法得到可资临床应用的足够预测值,因此,在直肠癌患者进行新辅助放化疗后,如欲对其病理完全缓解情况进行预测,不宜通过PET扫描和CT扫描进行。

10.1097/SLA.0b013e318277b625
PMC:
PMID:
Neither FDG-PET Nor CT Is Able to Distinguish Between a Pathological Complete Response and an Incomplete Response After Neoadjuvant Chemoradiation in Locally Advanced Rectal Cancer: A Prospective Study
Guillem, Jose G. MD *; Ruby, Jeannine A. MD *; Leibold, Tobias MD *; Akhurst, Timothy J. MD +; Yeung, Henry W. MD +; Gollub, Marc J. MD +; Ginsberg, Michelle S. MD +; Shia, Jinru MD ++; Suriawinata, Arief A. MD ++; Riedel, Elyn R. MA [S]; Mazumdar, Madhu PhD [S]; Saltz, Leonard B. MD ||; Minsky, Bruce D. MD [P]; Nash, Garrett M. MD *; Paty, Philip B. MD *; Temple, Larissa K. MD *; Weiser, Martin R. MD *; Larson, Steven M. MD +
Objective: To prospectively compare the ability of flourodeoxyglucose-positron emission tomography (FDG-PET) and computed tomography (CT) to identify a pathological complete response (pCR) in patients with rectal cancer treated by chemoradiation. Background: A major obstacle in pursuing nonoperative management in patients with rectal cancer after chemoradiation is the inability to identify a pCR preoperatively. Methods: A total of 121 patients with rectal cancer were prospectively enrolled. FDG-PET scans and helical CT scans were obtained before and after neoadjuvant chemoradiation. Consensus readings of PET and CT scans were used to classify certainty of disease (5-point confidence rating scale). The ability of PET and CT scans to accurately distinguish a pCR (ypT0) from an incomplete response (ypT1-4) was estimated using the area under the receiver operating characteristic curve (AUC). Results: Of the 121 patients, 26 (21%) had a pCR. PET and CT scans were equally inadequate at distinguishing a pCR from an incomplete response (AUC = 0.64 for both, P = 0.97). Among the 26 patients with a pCR, 14 (54%) and 5 (19%) were classified as complete responders on PET and CT scans, respectively. Among the 95 patients with an incomplete pathological response, 63 (66%) and 90 (95%) were classified as incomplete responders on PET and CT scans, respectively. None of the individual PET parameters, including visual response score, mean standard uptake value (SUVmean), maximum SUV (SUVmax), and total lesion glycolysis, accurately distinguished a pCR (AUCs = 0.57-0.73). Conclusions: Neither PET nor CT scans have adequate predictive value to be clinically useful in distinguishing a pCR from an incomplete response and, therefore, should not be obtained for the purpose of attempting to predict a pCR after neoadjuvant chemoradiation for rectal cancer.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
66
#放化疗#
69
#PET#
71