Dig Dis Sci: 晚期慢性肝病患者肝静脉压力梯度≤10mmHg与临床结果相关
2022-02-25 MedSci原创 MedSci原创
肝静脉压力梯度 肝静脉压力梯度(HVPG):经颈静脉插管测定肝静脉锲入压与游离压,两者之差即为HVPG,反映门V压力的大小。正常HVPG10mmHg则为门静脉高压。
肝硬化的临床病程主要由门静脉高压的进行性加重、高动力循环、细菌易位和全身炎症的激活决定。临床失代偿(CD)与这些机制的进展有关,可以通过血流动力学或临床特征来识别。CD 定义为出现静脉曲张出血、腹水、黄疸或脑病中的至少一种,每年发生率为 4-12%。确定 CD 的预测因子很重要,因为肝硬化中的死亡与 CD 的发展显著有关。众所周知,腹水、静脉曲张和静脉曲张出血的发展需要肝静脉压力梯度(HVPG)> 10mmHg(定义为临床上显着的门静脉高压症,CSPH)。HVPG 从基线降低 10-20% 或降至 <12 mmHg可能可以降低死亡或肝移植的风险。在本研究中,研究人员旨在判断 HVPG≤10 mm Hg 肝硬化患者的自然病程、CD 模式和临床结果。

研究人员将患有晚期慢性肝病 (aCLD) [组织学肝硬化 ( n =196) 或肝硬度测量 (LSM) > 15 kPa ( n = 65)] 和 HVPG 6-10 mmHg 的患者纳入本项研究。主要观察目标是研究他们的自然病程的变化和CD 模式的差异。为此,研究人员还分析了就诊时 CD 的预测因素以及对卡维地洛的反应差异。
在 HVPG 6-10 mmHg 的 261 名患者中,129 名(49.4%)在首次就诊时患有CD;最常见的 CD 表现是腹水 ( n = 77) 和黄疸 ( n = 65)。基线 HVPG ≥ 8 mmHg 与更大的 CD 风险独立相关 [HR:1.7;p =0.002,AUROC:0.85(95%CI-0.81–0.91)]。14.4% 的代偿期患者会出现新 CD症状(中位持续时间为 23.1 个月)。尽管基线 HVPG 相当,但发生新 CD 的患者在随访中具有更高的 HVPG(15.3±3.7 VS 8±2.1 mmHg;p < 0.001)。基线 LSM > 26.6 kPa、门体分流和血清白蛋白独立预测新 CD。对卡维地洛的总体 HVPG 反应(n = 60) 为 23.3%,与基线 CD 和 HVPG 无关。
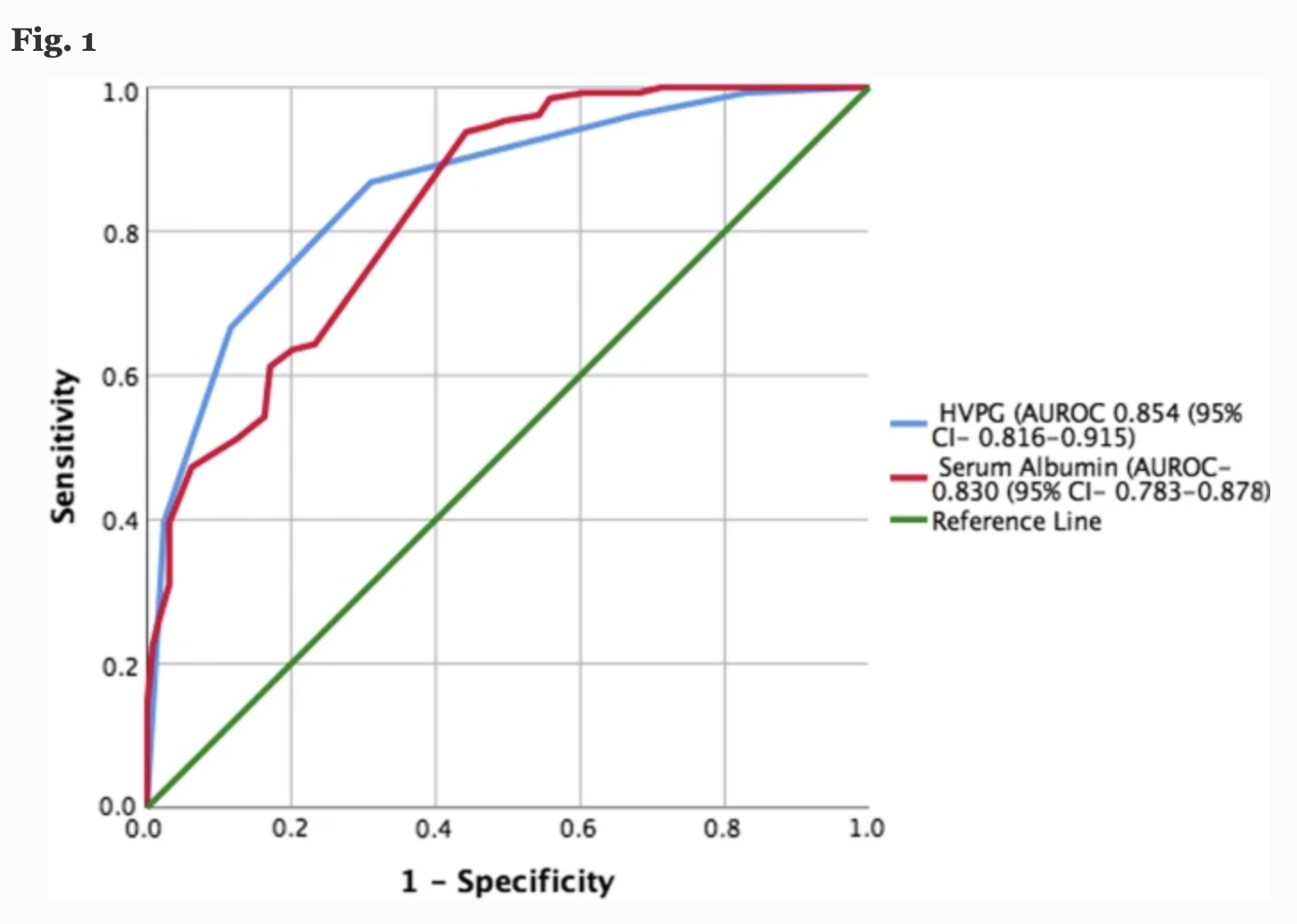
图:肝静脉压力梯度的ROC曲线
本项研究结果证实近一半 HVPG 6-10 mmHg 的患者患有 CD。降低 HVPG≥8 mmHg 患者门静脉压力的干预措施可能会改善长期预后。
原始出处:
Ankur Jindal. Et al. Clinical Outcomes in Patients with Advanced Chronic Liver Disease and Hepatic Venous Pressure Gradient ≤ 10 mm Hg. Digestive Diseases and Sciences.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
51
#临床结果#
51
#肝病患者#
63
#静脉#
50
学习学习
66