AIM:年轻型大肠癌发病率增高
2011-12-14 MedSci原创 MedSci原创
美国国家癌症数据库的研究结果表明,,50岁以下成年人的大肠癌(CRC)发病率在过去10年内增加了2.1%。美国安德森肿瘤研究中心的Yi-Qian Nancy You博士等近日也在《内科学文献》(Archives of Internal Medicine)上发表论文称,年轻型CRC的中位发病年龄为44岁,其中75.2%在40岁至49岁发病。 研究者在1998年1月至2007年12月之间对64068
美国国家癌症数据库的研究结果表明,,50岁以下成年人的大肠癌(CRC)发病率在过去10年内增加了2.1%。美国安德森肿瘤研究中心的Yi-Qian Nancy You博士等近日也在《内科学文献》(Archives of Internal Medicine)上发表论文称,年轻型CRC的中位发病年龄为44岁,其中75.2%在40岁至49岁发病。
研究者在1998年1月至2007年12月之间对64068名浸润性结肠癌和直肠癌的年轻患者(年龄小于50岁)进行了研究,发现直肠癌的发病率增长更快,其年度变化百分比(APC)为3.9%,95%可信区间CI为3.1%至4.7%,而结肠癌APC为2.7%,95% CI为2%至3%。这些数据与50岁以上人群的大肠癌发病率下降形成了鲜明对比。
研究表明,地理因素、种族差异、以及经济水平都对CRC的发病率有影响。
作者称,与老年型CRC相比,年轻型CRC在非白人中发病率更高(17.6%比29.5%,P<0.001),没有保险和医疗补助者发病率高于有保险和医疗补助者(16.5%比4.7%,P<0.001),美国南部发病率高于西部(56.2%比50.3%,P<0.001)。
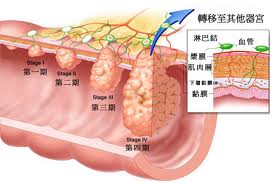
此外,晚期大肠癌(III期和IV期)在年轻人中更为常见,结肠癌为63%,直肠癌为57%。研究者还发现晚期大肠癌的独立危险因素之一为年龄较小:
30至39岁者与40至49岁者相比:风险比HR为1.21,95% CI为1.1至1.4;
18至29岁者对40至49岁者相比:HR为1.4,95% CI为1.2至1.6。
种族也是一个独立危险因素,非裔美国人同美国白人相比HR为1.2,95% CI为1.1至1.3。
有无保险是另外一个危险因素:
没有保险者与有保险者相比:HR为1.2,95% CI为1.1至1.3;
没有医疗补助者与有医疗补助者相比:HR为1.6,,95% CI为1.5至1.8。
作者称,关于年轻型CRC仍有很多未明确的危险因素,包括直肠出血、腹痛和肠型改变等,可能使医生忽略CRC的一些非特异性症状,导致漏诊或误诊。(生物谷bioon.com)
Young-Onset Colorectal Cancer: Is It Time to Pay Attention?
Y. Nancy You, MD, MHSc; Yan Xing, MD, PhD; Barry W. Feig, MD; George J. Chang, MD, MS; Janice N. Cormier, MD, MPH.
The 2010 Annual Report to the Nation on Cancer celebrated a steady decline in the incidence of colorectal cancer (CRC).1 This progress has been largely attributed to CRC screening, recommended for adults 50 years or older since 1996.2 In sharp contrast to overall trends, the incidence of CRC appears to be increasing among adults younger than 50 years,1, 3 a group for whom average-risk screening is not routine. Particularly concerning is a trend toward advanced-stage CRCs,1, 3 suggesting a potential role for increased clinical vigilance and more prompt evaluation of symptomatic patients. To raise clinical awareness and facilitate recognition, we undertook a cohort study to (1) examine incidence trends; (2) define the distinct clinicopathologic manifestations of young-onset CRC; and (3) identify risk factors for advanced-stage disease.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#癌发病率#
63
#发病率#
62
#癌发病#
65
#增高#
68
#增高#
75