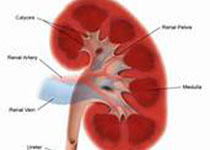
J Gastroen Hepatol:胃酸抑制剂与肾病风险研究
2018-08-13 zhangfan MedSci原创
研究认为,质子泵抑制剂治疗与急性间质性肾炎、急性肾损伤、慢性肾病以及终末期肾病风险增加相关,而组胺2受体拮抗剂治疗不会导致上述肾脏疾病风险增加
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
68
#风险研究#
72
#酸抑制#
84
#GAS#
54
#AST#
69
#EPA#
62
很有趣的研究啊~看来临床上还是需要有所注意啊
87