20世纪90年代,多项临床研究显示,支架在处理冠状动脉急性闭塞、预防再狭窄方面明显优于单纯球囊扩张术。同时在迈入21世纪以来,药物洗脱支架的面世,进一步降低了再狭窄的发生率。
近年来,随着医疗技术的发展,为经皮冠状动脉介入治疗技术带来了新的希望。然而,充分了解支架的结构和植入技术是保证手术成功的关键因素。本文对其关键点进行汇总,分享给各位同道。
一、冠状动脉支架和分类和适应症
冠状动脉支架能有效地处理夹层,提供机械支撑并减轻弹性回缩。 冠状动脉支架的分为:裸金属支架、药物洗脱支架和生物可吸收支架。药物洗脱支架面世之后,支架内再狭窄的发生率明显低,适应症范围进一步扩大。然而,值得注意的是,药物洗脱支架面临着内皮修复缓慢,血栓形成,需要长期服用抗血小板药物,可能诱发动脉瘤形成等一系列问题。
从冠状动脉支架出现以来,其适应证范围不断拓宽,包括从用于处理急性闭塞并发症到预防再狭窄,从大血管病变到小血管病变,从病情稳定、无血栓形成的择期介人治疗到急性心肌梗死患者等等。具体而言,适用的情况包括:
1,慢性稳定型冠心病:病变直径狭窄≥90%;病变直径狭窄<90%伴有相应缺血证据或血流储备分数≤0.8,如左主干直径狭窄>50%;前降支近段直径狭窄>70%;2支或3 支冠状动脉直径狭窄>70%且左心室功能受损(左心室射血分数<40%);大面积缺血(缺血面积>左心室10%);单支通畅冠状动脉直径狭窄>50%;任一冠状动脉直径狭窄>70%,表现为活动诱发的心绞痛或等同症状,并对药物治疗反应欠佳。
2,非 ST 段抬高型急性冠状动脉综合征:根 据患者的病史、症状、体征、血流动力学、心电图、肌钙蛋白、GRACE 评分进行风险分层,建议极高危者、高危和低危 者分别行紧急(2h 以内)、早期(24h 以内)和择期血运重建。参照慢性稳定型冠心病支架植入的标准,如冠状动脉病 变解剖结构适合植入支架,可行冠状动脉支架植入术。
3,急 性 ST 段抬高型心肌梗死(STEMI):第一,直接 PCI 治疗:发病 12 小时 内的 STEMI 患者;院外心搏骤停复苏成功的 STEMI 患者;存在提示心肌梗死的进行性心肌缺血症状,但无 ST 段抬高, 出现以下一种情况(血液动力学不稳定或心源性休克;反复 或进行性胸痛,保守治疗无效;致命性心律失常或心搏骤停;;机械并发症;急性心力衰竭;ST 段或 T 波反复动态改变,尤其是间断性 ST 段抬高)的患者;STEMI 发病超过 12 小时, 但有临床和/或心电图进行性缺血证据;伴持续性心肌缺血 症状、血液动力学不稳定或致命性心律失常。 第二,急诊或 早期冠状动脉造影:院外不明原因心搏骤停心肺复苏成功, 但未确诊为 STEMI 的患者,如高度怀疑有进行性心肌缺血, 宜行急诊冠状动脉造影;胸痛自发性或含服硝酸甘油后完全 缓解,抬高的 ST 段恢复正常,尽管无症状再发或 ST 段再度 抬高,建议早期(<24 小时)行冠状动脉造影。第三,溶栓 后 PCI:溶栓失败的患者应立即行紧急补救 PCI;溶栓成功 的患者应在溶栓后 2~24 小时内行 PCI。
二、支架植入技术要点
1,指引导管的选择
支架植入术对指引导管的选择与球囊扩张术相似,但对支撑力要求更高,这对病变近段血管迂曲、成角病变、远端血管病变及长节段病变植入长支架时尤为重要。对指引导管直径的选择首先必须能够容纳拟植入的支架顺利通过,同时考虑血管起始部直径及有无斑块,病变血管对支撑力的要求、术者的经验及对指引导管的控制能力、是否需要双球囊对吻扩张等因素综合决定。
2,导引导丝的选择
导丝的选择及操作在很大程度上决定了介入手术是否能够取得成功,也是冠脉介入术者需要掌握的基本技能。导引导丝应该具有良好的支撑力和调控性能,同时应尽可能的将导丝送至病变血管的最远端,以增加支撑力。但对于严重弯曲的血管而言,可尝试送入两条导丝增强支撑力。
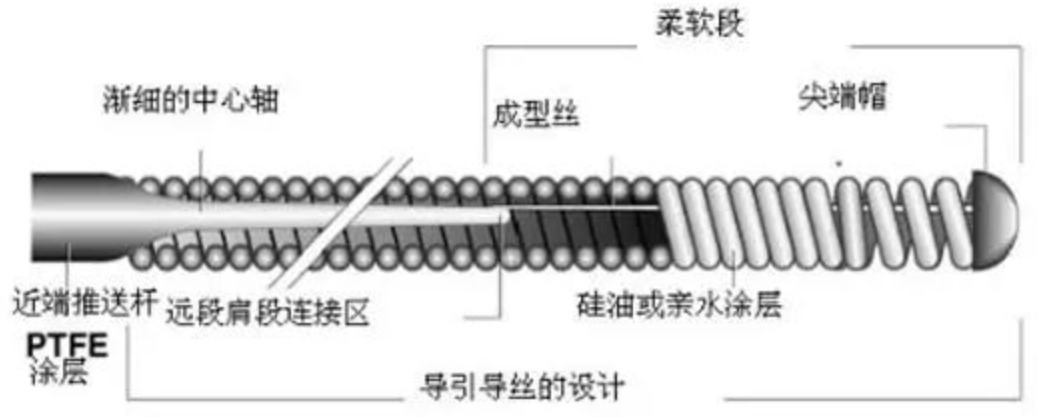
导丝结构
值得注意的是,有些导丝尖端较硬,使用时应尽量避免进入夹层甚至造成血管穿孔。
3,球囊预扩张
病变狭窄严重、迂曲成角、钙化时,为了减少支架前进的阻力、避免支架脱落,一般应进行预扩张。预扩张球囊通常比靶病变血管直径小0.5mm。球囊不能扩张的病变不适合植入支架。
对严重钙化病变可先行旋磨,然而再酌情植入支架。当病变狭窄不是很严重的情况下,有经验者可以不经球囊预扩张而直接植入支架。
4,支架选择
在选择支架时,需要综合考虑支撑力、柔软度、对分支的影响,在病变及其近端血管弯曲不明显、病变处无重要分支发出时以选择管状支架为主,在病变附近有大分支时,应选择网孔较大的管状支架以便必要时,可对分支进行扩张。在病变成角明显或近端血管弯曲严重时,宜选用缠绕支架等柔软度很高的支架。
支架直径的判断,要考虑到病变近端和远端血管的直径、释放系统的顺应性,一般以支架与血管直径之比为1.1:1为宜,使用药物洗脱支架时建议完全覆盖病变血管段。
5,支架植入前的准备
植入支架前的准备有不同的方式,并无统一规定。应先洗净手套上的血迹,最好不要过多接触支架本身。确认尺寸无误,冲洗释放系统的导丝腔,用湿纱布擦洗导引钢丝。支架到位前最好不要对释放系统的球囊腔抽吸负压以免破坏支架与球囊壁之间的紧密接触。另外,对不太熟悉的支架在准备时还应留意标记与支架两端边缘的距离。
6,支架的植入
支架通过Y型连接器时应将Y连接头止血阀充分放开,使支架通过时无任何阻力。在导管内推送支架时应尽量平稳、力量均匀,在支架被送出指引导管前应先确定指引导管确在冠状动脉内,然后固定指引导管、导丝,平稳地将支架送到病变处。
在支架释放前,应确认支架定位是否满意,一旦偏心或者有螺旋形撕裂的病变,应行多个角度投照。同时应尽量减少支架在血管内的大幅度往返移,特别是血管严重弯曲、成角、钙化时,以免造成支架的脱落,栓塞和急性血管闭塞。
在确定最佳位置后,用装有少量稀释造影剂的10ml或20ml注射器抽吸负压,连接加压泵,再次确认支架位置,迅速充盈球囊,将支架置于病变处。在使用药物洗脱支架时,不主张移动球囊位置进行往后扩张,如果支架两端血管直径相差较大,应换用较大直径的短球囊对血管较粗的一端进行后扩张。
7,同一血管植入多个支架时的顺序
如果长节段病变需要植入多个支架时,应先远后近,尽量避免穿过近端支架再植入远端支架,除技术上难度较大外,有时可能会损伤其中一个甚至同时损伤两个支架,或造成急性血管闭塞等严重后果。
8,支架植入后球囊后扩张
支架植入后球囊后扩张应选择非顺应性耐高压球囊,球囊与血管比例(1.0-1.1):1,压力多选择14~16atm,冠状动脉血管内超声(IVUS)对确定血管腔的真正大小、指导支架植入后的高压力球囊后扩张及判定支架植入效果有一定帮助。
看起来简单的支架植入的过程,实际上整个过程惊心动魄,医生要冷静应对各种可能出现的情况。同时,随着经皮冠状动脉介入治疗不断发展,新器械、新技术将不断涌现,未来在冠心病的治疗上将取得更进一步的疗效。
参考资料
1.冠状动脉球囊成形术与支架植入术操作规范(2022 年版)
2.冠心病介入治疗第8版.人民卫生出版社
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#支架植入#
88
学习
53
#冠脉支架#
94
进一步学习了
58
#植入#
60
#支架植入术#
0