Front Oncol:徐兵河院士团队发现HER2-乳腺癌中HER2低表达可能是预后良好指标
2022-01-17 yd2015 MedSci原创
研究表明,HER2-low肿瘤一种临床特征鲜明的类型,尤其是在HR阳性亚群中,并且可能是HER2-乳腺癌患者预后良好指标。
2022年1月17日,Frontiers in Oncology杂志上发表了一项徐兵河院士为通信作者的研究成果,主要是探索在HER2-乳腺癌患者中HER2-低表达(HER2-low)患者的临床病理特征以及临床预后。
研究筛查2005年至2015年期间的2202例患者,最终纳入1433例患者,其中618例(43.1%)为HER2-low肿瘤,815例(56.9%)为HER2- 0肿瘤。在618例HER2-low肿瘤患者中,454例(31.7%)为HER2 IHC 1+, 164例(11.7%)为HER2 IHC 2+。当按HR状况分层时,1045例(72.9%)患者为HR阳性患者,388例(27.1%)为三阴性患者。
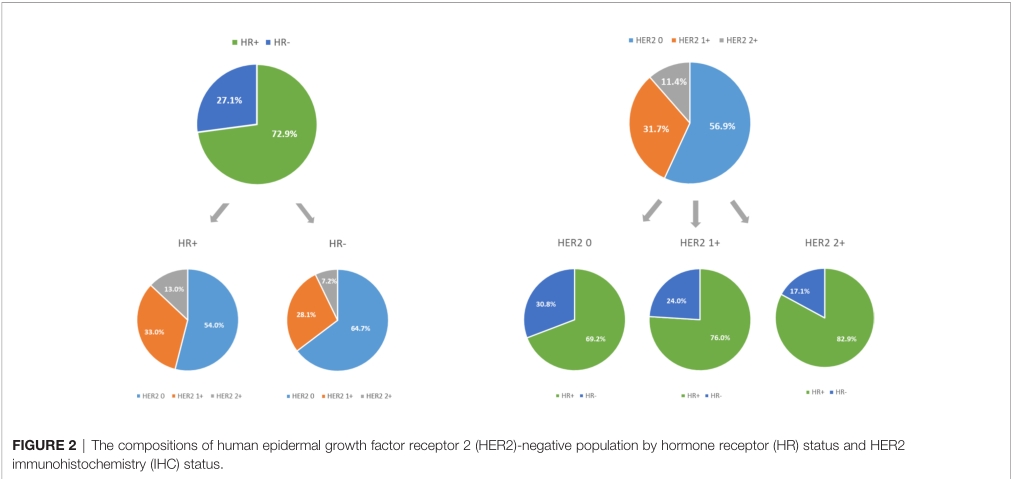
与HER2-0患者相比,HER2-low患者HR阳性的比例更高(p<0.001)。 HER2 IHC 2+患者比例最高(82.9%), 其次是HER2 IHC 1+患者(76.0%)。HR阳性患者中HER2-low患者比例较HR阴性患者的高。HR阳性患者中HER2 IHC 1+和IHC 2+患者的比例分别为33.0%和13.0% ,而在HR阴性患者中分别为28.1%和7.2% (p <0.001)。
整个人群的中位随访时间为62.6个月(95% CI: 58.0-67.1)。HER2- low的转移性乳腺癌患者的生存期明显较HER2- 0患者延长(48.5个月vs. 43.0个月,p = 0.004);在HR阳性患者中,也观察到类似的趋势 (54.9个月 vs. 48.1个月s, p = 0.011);但是在HR阴性患者中,没有显著的统计学差异(29.5个月 vs. 29.9个月, p =0.718)。
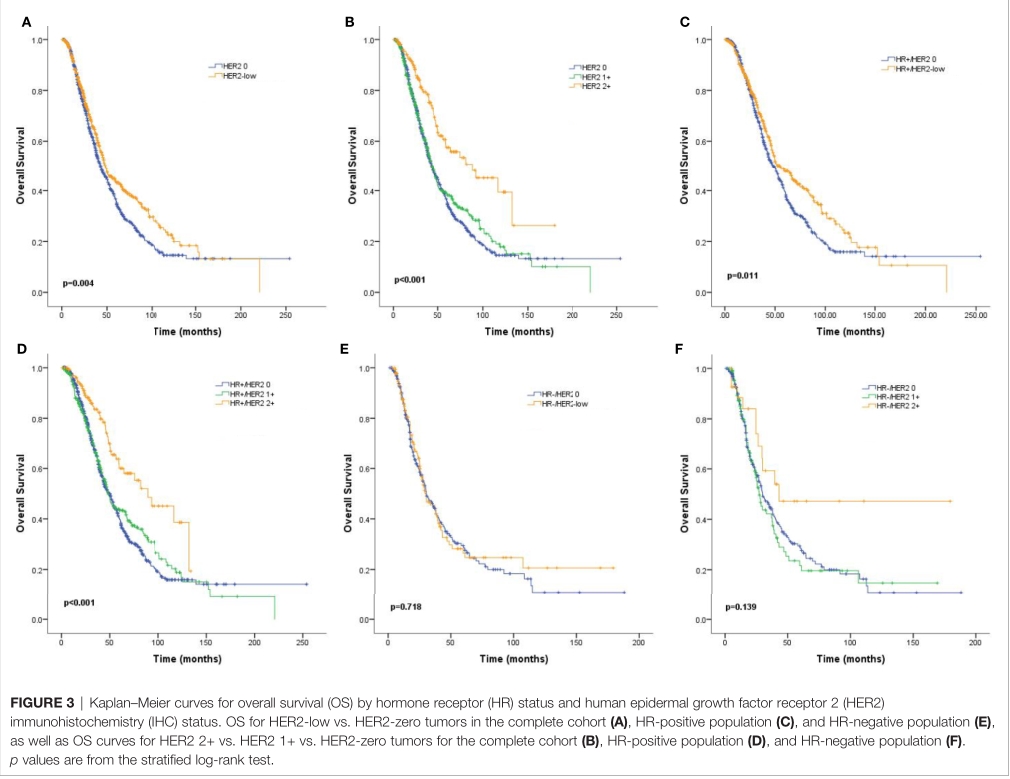
更具体地说,在整个患者群体中,HER2 IHC 2+患者比HER2 IHC 1+和HER2- 0患者的OS更好(88.5个月vs. 43.6个月vs. 43.0个月,p<0.001);在HR阳性患者中也观察到类似的趋势 (88.5 个月 vs. 47.7 个月 vs. 48.1 个月,p < 0.001);但是在HR阴性患者中,没有显著的统计学差异(42.9个月 vs. 27.2个月 vs. 29.9个月, p = 0.139F)。
亚组分析显示,非内脏转移患者(HR: 0.70, 95% CI: 0.56, 0.88, p = 0.002)和HR阳性患者(HR: 0.81, 95% CI: 0.68, 0.96, p = 0.013)的OS有显著差异。
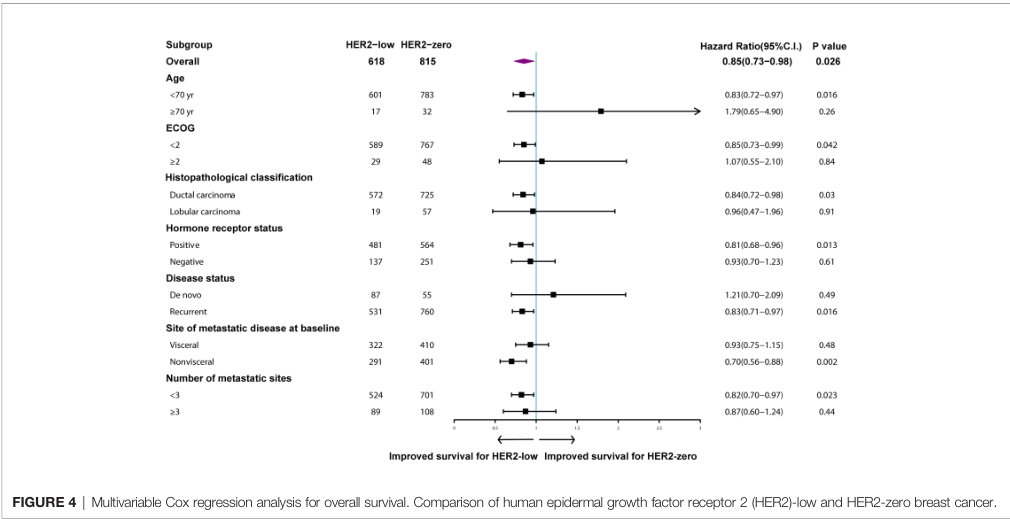
在HER2阴性患者中,HER2-low肿瘤被证实与良好OS独立相关(HR: 0.85, 95% CI: 0.73 0.98, p = 0.026),而HR阳性肿瘤(HR: 0.60, 95% CI: 0.51-0.70, p<0.001),更好的体能状态(HR: 0.75, 95% CI: 0.56-0.99, p = 0.039),较少转移部位(HR: 0.55, 95% CI: 0.46 0.67, p<0.001)与OS改善显著相关。

综上,研究表明,HER2-low肿瘤一种临床特征鲜明的类型,尤其是在HR阳性亚群中,并且可能是HER2-乳腺癌患者预后良好指标。
原始出处:
Li Y, Abudureheiyimu N, Mo H, Guan X, Lin S, Wang Z, Chen Y, Chen S, Li Q, Cai R, Wang J, Luo Y, Fan Y, Yuan P, Zhang P, Li Q, Ma F and Xu B (2022) In Real Life, Low-Level HER2 Expression May Be Associated With Better Outcome in HER2- Negative Breast Cancer: A Study of the National Cancer Center, China. Front. Oncol. 11:774577. doi: 10.3389/fonc.2021.774577
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
64
#HER2-#
94
#徐兵河#
75
#良好指标#
81
学习#学习#
72