NEJM:无导线起搏器临床证实安全有效,阜外医院心律失常中心参与其中
2015-12-30 赵爽 365医学网
近日,国家心血管病中心阜外医院心律失常中心张澍团队参与的无导线起搏器全球临床研究结果发表于新英格兰医学杂志上,该研究是一项前瞻性、非随机、多中心、上市前研究, 纳入了来自全球19个国家,56个中心的725例患者,其中719例患者成功植入无导线起搏器,成功率高达99.2%。所有患者均符合单腔心室起搏器(VVI)的植入适应证,包括房颤伴慢心室率(64%),窦房结功能障碍(17.5%),房室传导
该研究的目的是评估Micra经导管无导线起搏系统的安全性及有效性。研究通过术后6个月是否会发生与无导线起搏系统相关及手术相关的不良事件来评估其安全性,通过术后6个月随访时是否具有低(电压≤2V,脉宽0.24ms)并且稳定(植入后输出增加<1.5V)的起搏阈值来评估其有效性。
无导线起搏器是集脉冲发生器与起搏电极于一体的新型起搏器,无需静脉植入心内膜导线,而是以微缩胶囊的形式植入患者的心腔内,因此也无需皮下切口和囊袋。这种无导线起搏器如子弹头大小,体积为0.8cm3,直径 6.7 mm,长25 mm,重量 2 g,体积和重量为传统起搏器的十分之一,其功能却与传统的心室单腔起搏器无异,同样具有频率应答及自动阈值管理等功能。术中通过穿刺股静脉,经专门的递送系统送入无导线起搏器并于右心室释放,待确定装置头端的四个爪形结构稳定的固定于心室肌后,断开栓绳并撤出递送系统。
术后6个月的随访结果显示主要的有效性和安全性终点分别为96%(基于永久性起搏器数据所设定的有效性目标为83%)和98.3%(基于永久性起搏器数据所设定的安全性目标为80%)。共有25例患者共发生过28例不良事件,主要包括心脏穿孔、心衰、血栓形成等。不良事件发生率明显少于传统的永久性起搏器(4.0% vs. 7.4%; HR, 0.49; 95% CI, 0.33-0.75; P=0.001);此外住院事件(2.3% vs. 3.9%)和需进行植入后调整术的发生率(0.4% vs. 3.5%)也明显减少。患者植入无导线起搏器后起搏阈值会立刻降低并能保持长时间稳定。统计结果显示,植入后平均心室阈值为0.63V(脉宽0.24ms), R波11.2mV,导线阻抗为724Ω,6个月随访时平均阈值为0.54V(脉宽0.24ms), R波15.3mV,627Ω。91%的患者输出电压低于1.5mV(脉宽0.24ms)。基于6个月的随访结果,预计平均电池寿命12.5年,其中将有94%的患者电池寿命超过10年。
需要指出的是,该临床研究为非随机、对照研究,使其不能直接与传统的永久性起搏器相比较,而且目前Micra无导线起搏器只具备单腔心室起搏功能,随访结果仅限于6个月的临床数据,其长期安全性及有效性仍需进一步临床观察。该研究的最大意义是证明了无导线起搏器在人体内使用的安全性和可靠性。无导线起搏器操作简单、微创美观、无囊袋及导线并发症等优势必将推动其在临床上的广泛应用,为患者带来福音。
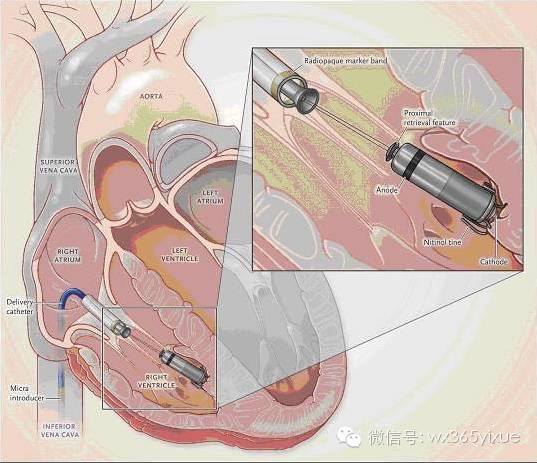
图1 Micra经导管无导线起搏器被植入右心室心尖部,起搏器近端通过栓绳与递送系统连接,远端通过四个爪形结构固定于心肌。
文献来源:
Reynolds D, Duray GZ, Omar R, Soejima K, Neuzil P, Zhang S, Narasimhan C, Steinwender C, Brugada J, Lloyd M, Roberts PR, Sagi V, Hummel J, Bongiorni MG, Knops RE, Ellis CR, Gornick CC, Bernabei MA, Laager V, Stromberg K, Williams ER, Hudnall JH, Ritter P; Micra Transcatheter Pacing Study Group.A Leadless Intracardiac Transcatheter Pacing System.N Engl J Med. 2015 Nov 9
小知识:无导线起搏器
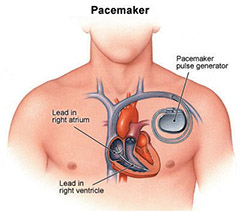
起搏器问世50年来在功能上发生了翻天覆地的变化,但导线加脉冲发生器的基本结构却从未改变,后者正是起搏器并发症的主要来源,包括导线断裂、脱位、心脏穿孔、导线路径中的静脉血栓、三尖瓣返流、放置脉冲发生器的囊袋感染和血肿等。因此,摒弃传统起搏器的导线成为近年起搏器技术发展的热点。
1. 经体表无线能量传输心脏起搏
1.1 超声能量传输方式
利用超声能量行心脏起搏的原理为在体表植入超声发射装置(发射器),通过静脉途径在心脏内植入超声接收装置(接收器),接收器可以接收发射器透过胸壁发送的超声能量并转换为电能量(即脉冲电流)进行心脏起搏。
2006年Echt DS等首先在猪模型上进行了无导线超声心脏起搏的可行性和安全性研究。2007年,Lee KL等利用相同的方法,首次在人体成功进行了通过超声能量进行心脏起搏的研究,该研究首次证实在人体利用超声能量行心脏起搏安全可行。2009年,Lee KL等在10例慢性心力衰竭患者中进行了利用超声能量进行左室起搏的研究。研究中测定起搏阈值为1.18±0.51V,并显示体位、呼吸等因素不会对超声信号的传导有显著影响。
2013年,Auricchio A等报道了3例利用这项技术在患者实现CRT的病例。3例患者分别植入利用超声能量起搏的左室无导线起搏系统(Wireless cardiac stimulation -LV system,WiCS-LV system),左室起搏阈值为0.7至1.0V。WiSE-CRT研究是评估利用超声能量行左室起搏实现CRT的一项临床研究,而此系统的有效性和安全性也有待这项研究结果的公布与证实。
1.2 磁能量传输方式
与利用超声能量相似,利用磁能量行心脏起搏是通过植入心前区皮下的发射器将磁能量传递至心腔内的电极接收器线圈,进而接收器将接收到的磁能量转换为交变电流,经整流和电容整形成为近似方波的心脏起搏脉冲进行心脏起搏。
2009年,Wieneke等首先报道了通过磁感应技术进行心脏起搏的方法,首次证实了通过体外电磁能量传输转换进行心脏起搏的可行性。2013年,Wieneke等进一步对利用磁能量进行心脏起搏的可行性进行了研究。结果显示发射器与接收器距离62-102mm范围内,均能实现起搏成功。影响磁能量消耗的主要因素是发射器与接收器的距离与起搏阈值。由于利用磁能量出现较晚,目前文献报道较少,且相关临床试验尚未开展。
2. 微型无导线起搏器
无论是利用超声还是磁能量,虽然都实现了无导线起搏,但仍然需要为能量的来源装置(发射器)制作囊袋。把电池整合入脉冲发生器的微型无导线起搏器,无疑能进一步减少囊袋带来的手术复杂性和相关并发症。另外,由于直接采用了传统电刺激的方法,因而也避免了间接的能量转换。微型无导线起搏器虽然起步较晚,却是目前商业化应用前景最广阔的无导线起搏器。
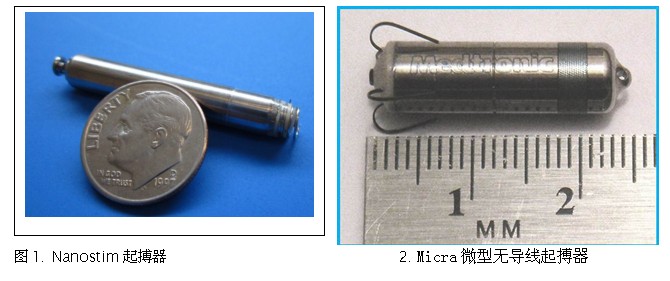
Nanostim起搏器是最早也是目前最成熟的微型无导线起搏器。起搏器呈棒状,大小约为7号电池,不及传统起搏器的1/10,见图1。由可操纵导管经股静脉植入到右心室心尖部行起搏功能,因此术后不仅不需要导线,而且不需要制作囊袋。此外,虽然Nanostim体积小,但寿命却长于普通起搏器,其在100%起搏时为9年,在50%起搏时可达13年。
Leadless研究(NCT01700244)是第一项测试Nanostim起搏器在人体安全性与可行性的临床试验。研究为前瞻性、单组、多中心研究。共入选33例患者,术中成功率为97%,平均植入时间44分钟。在2013年10月,Nanostim起搏器通过了欧盟标准认证并获准在部分欧洲国家上市,同时Nanostim公司也被St.Jude公司收购。2013年12月3日和5日,St.Jude公司分别公布了上市后在德国和法国的第一台Nanostim起搏器植入成功的报道。
与Nanostim起搏器类似,Medtronic公司也推出了自己的Micra微型无导线起搏器,见图2。针对Micra起搏器的Micra TPS研究于2013年12月9日在奥地利成功入选第一例患者并手术成功,初步随访结果预计于2014年下半年面世。
3.无导线起搏器的优势与不足
3.1 优势:可以避免导线相关的所有并发症。尤其是微型无导线起搏器,仅需经皮穿刺导管技术置入,操作简单、便捷,创伤小,无需外科手术制作囊袋,不影响患者外观,无起搏器囊袋的相关并发症。特别值得一提的是,通过无导线技术可以实现左室心内膜无线起搏并应用于CRT。
3.2 不足 ①.目前所有无导线起搏器均为心室单腔起搏(微型无导线起搏器)或双室起搏(左室仅有超声能量传输方式),尚无传统的DDD起搏模式。②.经体表无线能量传输的最大不足在于能量的损耗。③.目前无导线起搏器临床应用刚起步,对包括植入过程、起搏器是否脱落、感染后如何移除和临床效果等都需要今后大规模的临床研究验证。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









谢谢分享。
170
#阜外医#
79
不错,赞一个
156
这篇文章有一定深度
157
是一篇不错的文章
146
值得进一步关注
130
深奥
129
有点深哦
111
深奥
106
深奥
87