Aging Dis:年轻血液有益于年老患者缺血性卒中后的功能恢复
2017-10-08 MedSci MedSci原创
既往研究已经表明,血液中的物质可以大大逆转老化相关的损伤,因为研究发现老年小鼠暴露于年轻血液能够恢复成年干细胞的功能,改善小鼠认知,并可改善其心脏肥大。来自小鼠的全身因素也可以延长暴露于致死性治疗或疾病的伴侣的寿命。这些发现表明,健康的年轻伴侣的系统性环境可能对老年生物有益。然而,未知健康的年轻系统性环境是否可以改善缺血性卒中后的功能恢复。研究发现,与对照组相比,远端大脑中动脉阻塞(dMCAO)引
既往研究已经表明,血液中的物质可以大大逆转老化相关的损伤,因为研究发现老年小鼠暴露于年轻血液能够恢复成年干细胞的功能,改善小鼠认知,并可改善其心脏肥大。
来自小鼠的全身因素也可以延长暴露于致死性治疗或疾病的伴侣的寿命。这些发现表明,健康的年轻伴侣的系统性环境可能对老年生物有益。然而,未知健康的年轻系统性环境是否可以改善缺血性卒中后的功能恢复。
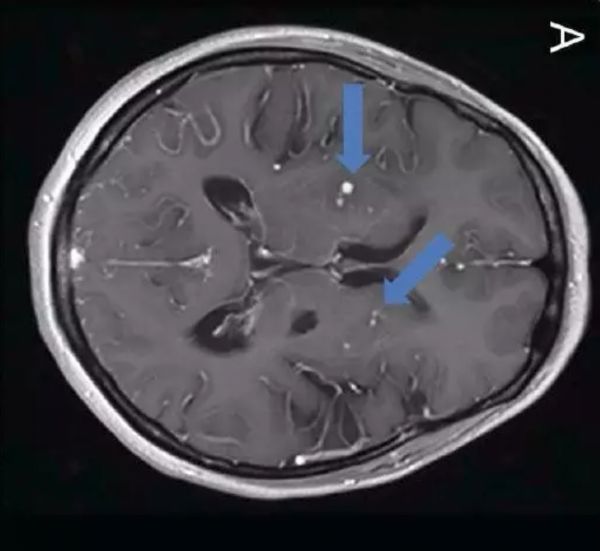
研究发现,与对照组相比,远端大脑中动脉阻塞(dMCAO)引起的缺血性卒中后老年大鼠腹腔内注射年轻血浆可以降低梗死体积和运动障碍。相反,年轻缺血性大鼠腹腔注射老年血浆会使脑损伤和运动缺陷恶化。使用蛋白质组学方法,研究人员发现老年大鼠血清中触珠蛋白的水平可明显升高,缺血性卒中年轻大鼠腹腔注射触珠蛋白可恶化其结局。
总之,该研究结果表明,老化的系统环境在缺血性卒中后的功能结局中起关键作用。
原始出处:
Mengxiong Pan, Peng Wang, et al., Aging Systemic Milieu Impairs Outcome after Ischemic Stroke in Rats. Aging Dis. 2017 Oct; 8(5): 519–530. Published online 2017 Oct 1. doi: 10.14336/AD.2017.0710
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
80
#年轻血液#
78
#缺血性#
68
#卒中后#
78
#缺血性卒#
77
#功能恢复#
92