Target Oncol:FLAURA中国研究表明一线奥希替尼治疗较吉非替尼改善中国人群EGFR突变NSCLC患者的预后
2022-02-14 yd2015 MedSci原创
FLAURA中国研究表明,一线奥希替尼治疗较吉非替尼改善中国人群EGFR突变NSCLC患者的预后。
在FLAURA的全球研究中,在EGFR突变阳性(EGFRm)的晚期非小细胞肺癌(NSCLC)患者中,与第一代EGFR TKIs相比,第三代EGFR-TKI奥希替尼显著提高患者的无进展生存期(PFS)和总生存期(OS)。因此,国内团队开展FLAURA中国研究,主要是评估中国人群中奥希替尼对比第一代EGFR-TKIs一线治疗EGFRm NSCLC患者的疗效。相关结果发表在Targeted Oncology杂志上。

FLAURA中国研究是一项双盲、随机、III期研究,纳入来自中国大陆的既往未治疗EGFRm(外显子19缺失或L858R)晚期NSCLC;136名患者被随机分配给奥希替尼(80 mg,每日1次;n = 71)或第一代EGFR TKI(吉非替尼或厄洛替尼;均选择了吉非替尼250mg 每日1次;n = 65)。患者被随机分配到治疗组,治疗直到疾病进展,不可接受的毒性,或撤回同意。主要终点是研究者评估的无进展生存期(PFS);OS是次要终点。
研究纳入136例患者,包括19例纳入全球研究患者和另外117例中国患者,其中71例接受奥希替尼治疗,65例接受吉非替尼治疗。
研究者评估奥希替尼组的无进展生存期(PFS)较吉非替尼组明显延长,中位PFS延长了8个月,分别为17.8个月(95% CI 13.6-20.7) vs 9.8个月(95% CI 8.3-13.8)(HR 0.56;95%CI 0.37-0.85;P =0.007)。

预后评估
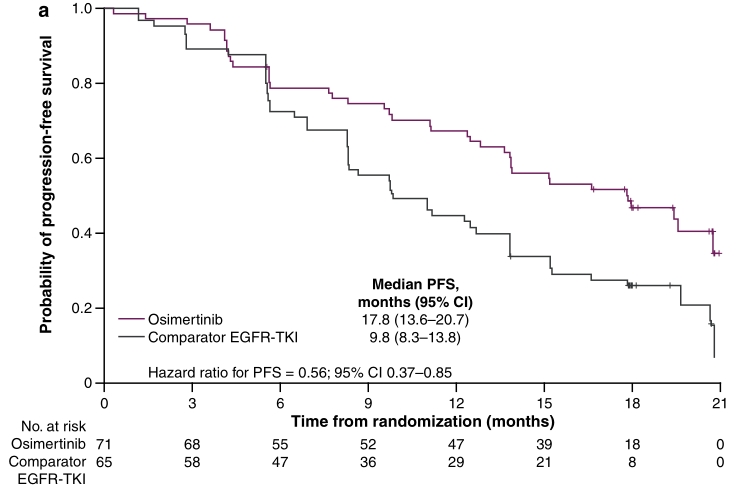
PFS
奥希替尼组和吉非替尼组的中位OS分别为33.1个月(95% CI 26.0-35.9)和25.7个月(95% CI 19.6-32.8),延长了7.4个月(HR 0.85;95%CI 0.56-1.29,P= 0.442)。

OS
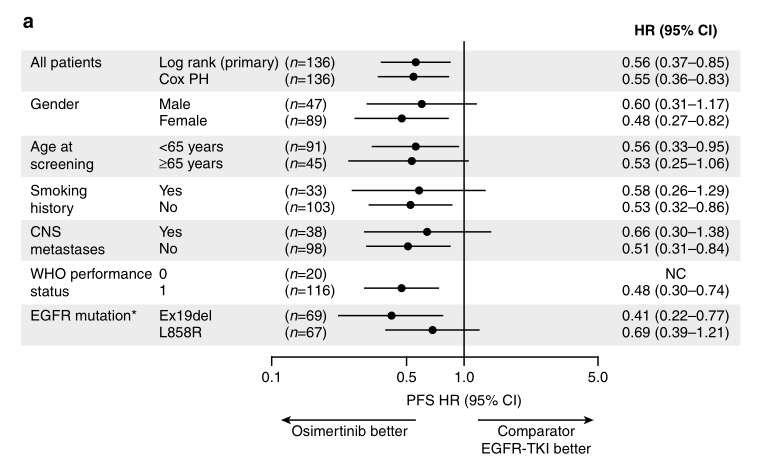
PFS亚组分析,几乎所有亚组患者均从奥希替尼组获益,但是OS亚组分析时,患者几乎不能奥希替尼组获益。

在奥希替尼组和吉非替尼组中,分别有54%和28%的患者报告了3级或3级以上不良事件(AEs),没有发现新的安全信号。

综上,FLAURA中国研究表明,一线奥希替尼治疗较吉非替尼改善中国人群EGFR突变NSCLC患者的预后。
原始出处:
Cheng Y, He Y, Li W, Zhang HL, Zhou Q, Wang B, Liu C, Walding A, Saggese M, Huang X, Fan M, Wang J, Ramalingam SS. Osimertinib Versus Comparator EGFR TKI as First-Line Treatment for EGFR-Mutated Advanced NSCLC: FLAURA China, A Randomized Study. Target Oncol. 2021 Mar;16(2):165-176. doi: 10.1007/s11523-021-00794-6. Epub 2021 Feb 5. PMID: 33544337; PMCID: PMC7935816.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
83
#target#
108
#SCLC患者#
93
#FLAURA#
86
#NSCLC患者#
95
#GFR#
76