本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


很多病人拿着HLA-B27的化验单会问到:我的HLA-B27是阳性,是不是就是强直性脊柱炎? 其实HLA-B27阳性不一定就是强直性脊柱炎; 大部分强直性脊柱炎的病人HLA-B27为阳性; 但大部分阳性的病人不一定是强直性脊柱炎。
目前有研究表明(Haroon N等3~4年的随访研究)只有不到30%的强直性脊柱炎(AS)患者出现较明显的脊柱骨化进展,有50%~60%的患者进展不明显,因此,寻找AS脊柱骨化的预测因素,对于判断疾病预后、以及干预治疗措施具有重要的意义。目前较为认可的AS骨化危险因素包括基线时骨化程度、基线时炎症水平以及吸烟。 炎症导致骨化一直存在争论,既往认为炎症与骨化不相关,首先是常用的抗风湿病药物,如甲氨
诺华(Novartis)近日宣布,单抗药物AIN457 (secukinumab)强直性脊柱炎2个关键III期研究(MEASURE-1,MEASURE-2)中均达到了主要终点和关键次要终点。这2个研究在近600例活动性强直性脊柱炎(AS)患者中开展,数据表明,与安慰剂相比,secukinumab显著改善了疾病的症状和体征,同时也显著改善了患者的身体机能和生活质量。该研究成果也标志着secukinu
众所周知,普通X线摄像技术局限于清晰度以及定量评分方法,很难对强直性脊柱炎(AS)的韧带骨赘生长进行评估。来自美国NIH的Sovira Tan等人利用CT扫描技术对AS韧带骨赘体积和高度进行定量评估,并探讨此方法的可靠性和效度。 该研究对38名AS患者进行腰椎CT扫描,并对其韧带骨赘体积和高度进行定量计算。为了评估此方法的可靠性,他们比较了来自2个机器同一天对9位AS患者扫描的结果。为了评估有效
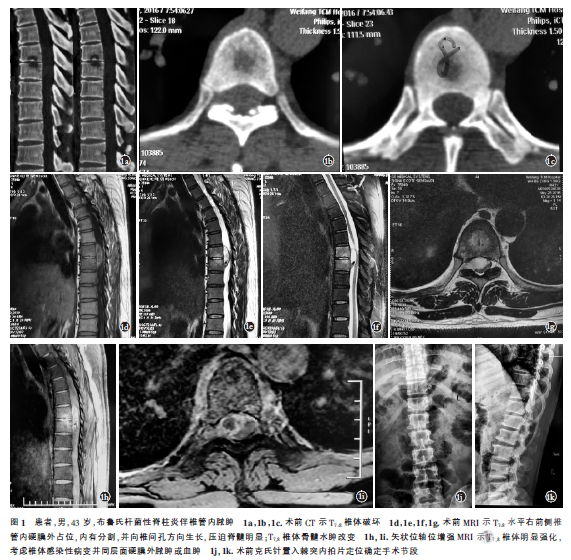
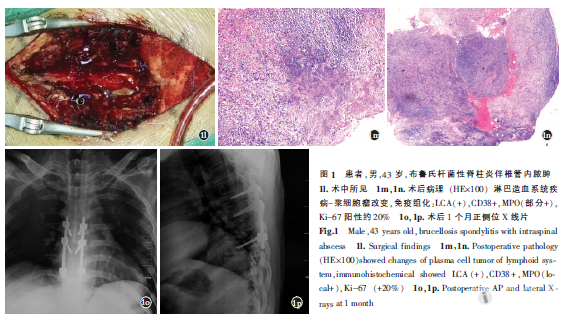
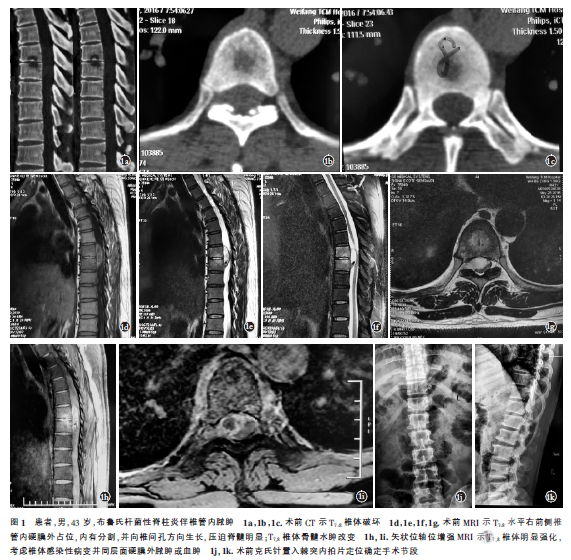
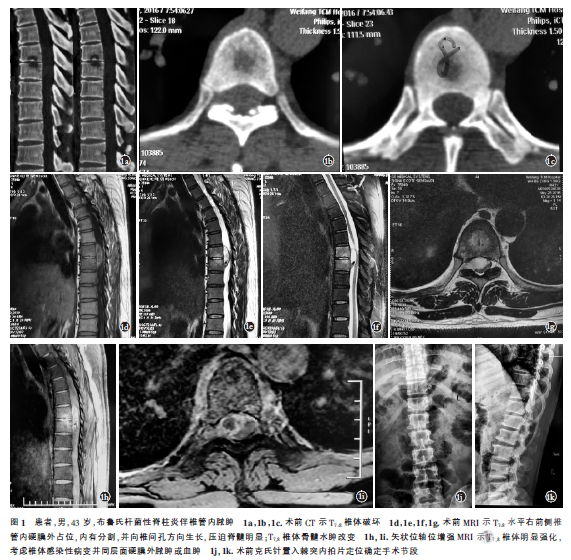
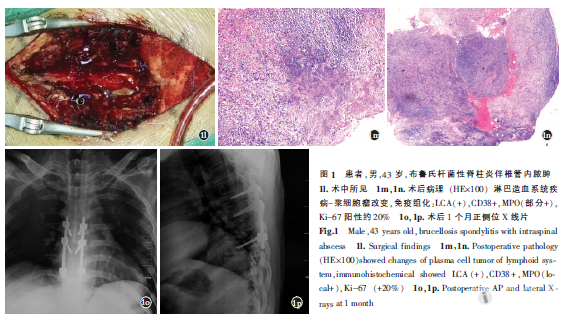
本期共刊出了3篇有关脊柱特殊类型感染的论著和综述,其临床意义值得关注。这些文章涉及脊柱结核和脊柱布氏杆菌病,这两种脊柱特殊类型感染的发病率呈逐年上升趋势,已经成为需要引起重视和观察研究的健康问题。以脊柱结核为例,虽然前些年我国肺结核发病率呈下降趋势,但受人口增加、人口老龄化、耐药菌、人类免疫缺陷病毒(HIV)传播等现状的影响,全球结核病卷土重来,骨关节结核患者数量呈明显上升趋势。骨与关节结核是最常


梅斯医学MedSci APP
医路相伴,成就大医
#硬膜外#
74
#脊柱炎#
77
#脓肿#
63
学习了受益匪浅
82
^_^^_^^_^^_^
81