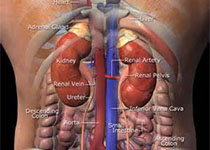
JCEM:肾上腺腺瘤患者的心脏代谢结局和死亡率
2021-07-13 MedSci原创 MedSci原创
在基于人群的队列中,肾上腺腺瘤与不良心脏代谢结局的患病率和发生率增加相关。
虽然肾上腺腺瘤与心血管发病率有关,但缺乏大规模的基于人群的数据。
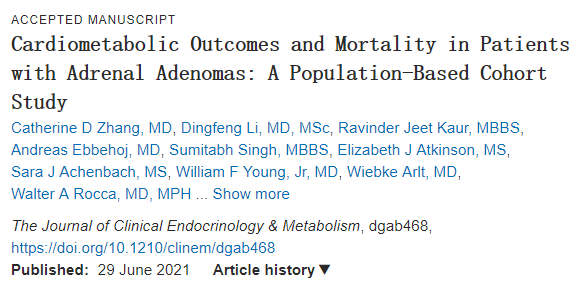
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在明确心脏代谢疾病的患病率和发病率,并评估基于人群的肾上腺腺瘤患者队列的死亡率。
 该研究为基于人群的队列研究,该研究的受试者为被诊断患有肾上腺腺瘤而没有明显激素过量的患者以及年龄和性别匹配的无肾上腺腺瘤对照者。该研究的主要结局指标为心脏代谢结局的患病率、发生率以及受试者死亡率。
该研究为基于人群的队列研究,该研究的受试者为被诊断患有肾上腺腺瘤而没有明显激素过量的患者以及年龄和性别匹配的无肾上腺腺瘤对照者。该研究的主要结局指标为心脏代谢结局的患病率、发生率以及受试者死亡率。

随访期间心脏代谢结局和死亡的累积发生率
1004名患者(58%为女性,中位年龄为63岁)被诊断出肾上腺腺瘤。在基线时,与对照者相比,肾上腺腺瘤患者更可能患有高血压(aOR为1.96,95%CI为1.58-2.44)、血糖异常(aOR为1.63,95%CI为1.33-2.00)、外周血管疾病(aOR为1.59,95%CI为1.32-2.06)、心力衰竭(aOR为1.64,95%CI为1.15-2.33)和心肌梗死(aOR为1.50,95%CI为1.02-2.22)。在6.8年的中位随访期间,肾上腺腺瘤患者比对照者更可能出现新发慢性肾病(aHR为1.46,95%CI为1.14-1.86)、心律失常(aHR为1.31,95%CI为1.08-1.58))、外周血管疾病(aHR为1.28、95%CI为1.05-1.55)、心血管事件(aHR为1.33、95%CI为1.01-1.73)和静脉血栓栓塞事件(aHR为2.15、95%CI为1.48-3.13)。两组受试者的调整后死亡率相似。
由此可见,在基于人群的队列中,肾上腺腺瘤与不良心脏代谢结局的患病率和发生率增加相关。
原始出处:
Catherine D Zhang.et al.Cardiometabolic Outcomes and Mortality in Patients with Adrenal Adenomas: A Population-Based Cohort Study.JCEM.2021.https://doi.org/10.1210/clinem/dgab468
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCE#
36
#肾上腺#
45
#JCEM#
44
临床上确实观察到了类似现象
78
#心脏代谢#
40
学习了
55