Cancer Cell:新型“液体活检”!非小细胞肺癌诊断准确率高达近90%
2017-08-17 MedSci MedSci原创
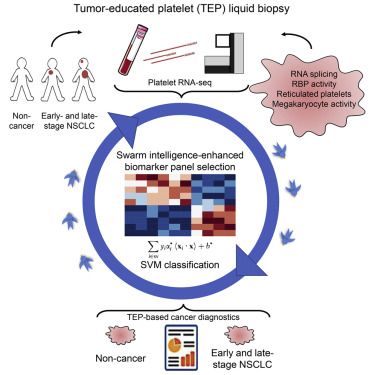
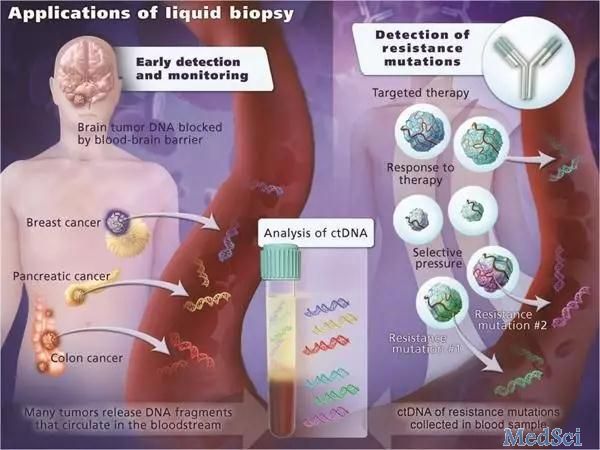
液体活检是近年来生物医学行业非常热门的领域之一。本周发表在Cell子刊上的一项研究描述了一种新型的液体活检。这一被称为thromboSeq的检测方法能够以近90%的准确率诊断出非小细胞肺癌。研究人员相信,这一技术已经足够强大到能开始临床试验了。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非小细胞#
72
#Cell#
75
#CEL#
64
#cancer cell#
75
#活检#
69