Gut:VAP-1可预测原发性硬化性胆管炎患者临床结局!
2017-04-21 xing.T MedSci原创
PSC患者VAP-1表达增加,促进肠道嗜淋巴细胞对肝脏内皮细胞的粘附,并且以底物依赖性的方式。并且循环形式的VAP-1水平升高可以预测患者的临床结局。
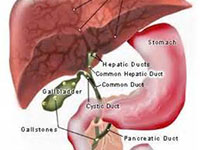
原发性硬化性胆管炎(PSC)是IBD的典型肝胆表现。该临床相关性与病理性粘膜T细胞募集到肝脏有关,通过血管粘附蛋白(VAP)-1-依赖的酶活性。近日,消化病领域权威杂志Gut上发表了一篇研究文章,研究人员旨在评估PSC患者胞外酶VAP-1的表达、功能和酶活性。
研究人员检测了VAP-1在PSC患者中的表达,并且评估了其表达水平与临床特征相关性,以及明确了采用特异性酶底物导致酶激活后对肝细胞的功能影响。
PSC患者肝内VAP-1酶活性增加,相比于免疫介导的疾病对照者和非肝病患者(P<0.001)。采用VAP-1抑制剂氨基脲处理后,在体外实验中,肠嗜α4β7+淋巴细胞对肝内皮细胞的黏附性降低了50%(P<0.01)。在自然的VAP-1底物实验中,可以被发炎的结肠上皮和肠道细菌所分泌的半胱胺的效率最高(酶产率最高),并且可以有效地诱导功能黏膜地址素细胞黏附分子在肝内皮细胞中的表达。在一个前瞻性评估的PSC患者队列中,升高的血清可溶性(s)VAP-1水平可以独立地(风险比为3.85,P=0.003)和加入肝硬化(风险比为2.02,P=0.012)后预测患者较差的无移植生存期。
PSC患者VAP-1表达增加,促进肠道嗜淋巴细胞对肝脏内皮细胞的粘附,并且以底物依赖性的方式。并且循环形式的VAP-1水平升高可以预测患者的临床结局。
原始出处:
Palak J Trivedi, et al. Vascular adhesion protein-1 is elevated in primary sclerosing cholangitis, is predictive of clinical outcome and facilitates recruitment of gut-tropic lymphocytes to liver in a substrate-dependent manner. Gut. 2017. http://dx.doi.org/10.1136/gutjnl-2016-312354
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#VAP#
87
#原发性#
76
#临床结局#
0
学习了,谢谢分享
110
学习了,谢谢分享
104
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。给点赞啦……
97
#原发性硬化性胆管炎#
68
#硬化性#
0
#胆管#
53