BMC Psychiatry:童年遭虐待,青春期出现行为问题几率较大!
2021-03-16 MedSci原创 MedSci原创
行为问题是指在童年和/或青春期表现出的反社会行为,包括行为障碍和对立违抗性障碍。行为问题基本特征为违抗、敌意、对立、挑衅、粗野、不合作和破坏行为,常在童年早期出现,青春期达到高峰。
行为问题是指在童年和/或青春期表现出的反社会行为,包括行为障碍和对立违抗性障碍。行为问题基本特征为违抗、敌意、对立、挑衅、粗野、不合作和破坏行为,常在童年早期出现,青春期达到高峰。行为问题在个人、家庭和社会负担中占有相当大的比例,并与心理健康和身体健康等多个领域产生负面结果。因此,深入了解导致行为问题的病因并制定有效的预防和干预措施至关重要。

近日,发表在BMC Psychiatry杂志一项研究显示,在11岁之前就遭受虐待的儿童,比在青春期遭受虐待更容易出现行为问题,如欺凌或偷窃。

在这项研究中,来自巴斯大学和布里斯托尔大学的研究人员对英国4岁-17岁的10648名儿童和青少年(男孩占51.6%)进行行为问题发展轨迹的探索,并调查了在发育过程中不同时间遭受的虐待与所衍生行为问题轨迹之间的联系。行为问题是在4岁、7岁、8岁、10岁、12岁、13岁和17岁时通过父母对孩子在过去六个月内的行为进行评分来衡量的。22岁时被要求报告身体,心理或身体状况。
研究人员确定了确定了四个发展轨迹:早期发作持续性行为问题(4.8%),青春期发作行为问题(4.5%),儿童期行为问题(15.4%)和低度(75.3%)行为问题。而且,在儿童期和青少年期出现行为问题的人群中,虐待更为常见。
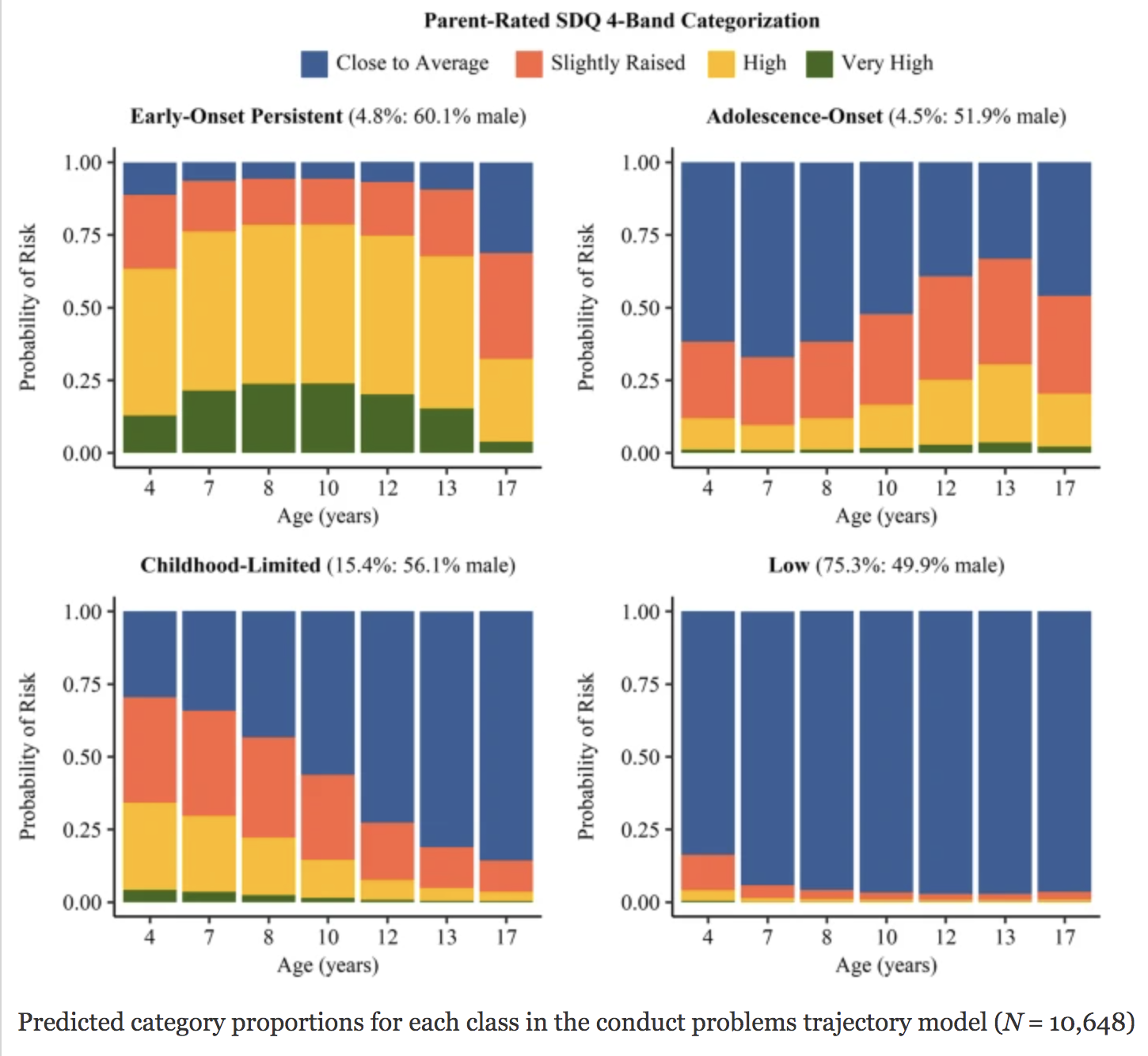
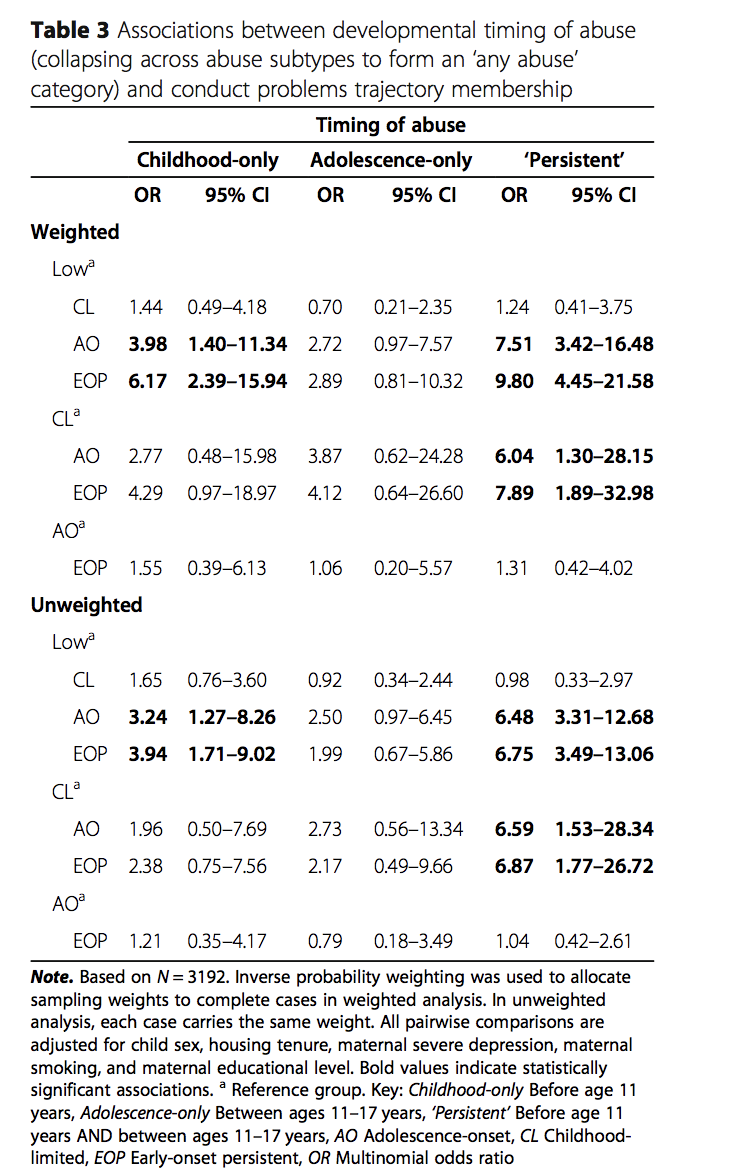
研究人员进一步发现,在童年和青春期遭受虐待,早期发作持续性行为问题的可能性高出10倍,在青春期出现行为问题的可能性高出8倍。在童年期遭受虐待,与早期发作持续性行为问题或青春期发生行为问题的风险增加4至6倍。相比之下,仅在青春期遭受虐待与出现严重行为问题没有显著相关性。
综上所述,虐待在有行为问题的年轻人的背景中更为常见,从青春期开始的行为问题可能与童年的不良经历有关,而可能不是青少年叛逆或同伴压力等。预防虐待儿童也可能有助于保护儿童不出现严重的行为问题。然而,必须指出的是,许多经历过虐待的年轻人可能并没有出现行为问题,而且没有虐待儿童也可能会出现行为问题。
原始出处
Bauer et al.Associations between developmental timing of child abuse and conduct problem trajectories in a UK birth cohort .BMC Psychiatry 2021, DOI: 10.1186/s12888-021-03083-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Psychiatry#
121
#BMC#
78
#青春期#
99
了解
128