ESC 2021丨FOURIER全新结果:依洛尤单抗显著降低ASCVD患者所有血管床急性动脉事件的风险
2022-02-17 “心关注”公众号 “心关注”公众号
动脉粥样硬化性心血管疾病(ASCVD)是一大类以动脉粥样硬化为病理基础的疾病的总称,包括冠心病、卒中和外周血管病等疾病。
动脉粥样硬化性心血管疾病(ASCVD)是一大类以动脉粥样硬化为病理基础的疾病的总称,包括冠心病、卒中和外周血管病等疾病。降低ASCVD的关键致病因素LDL-C可带来明确的心血管获益。大规模随机对照研究已经证实PCSK9抑制剂依洛尤单抗可强效降低LDL-C,显着降低心血管复合终点事件风险,但其对不同血管床的影响是否一致?
《心关注》特别邀请西安交通大学医学院第一附属医院袁祖贻教授为我们带来ESC 2021大会上发布的FOURIER研究最新分析结果,该研究证实依洛尤单抗可显着降低ASCVD患者所有血管床的急性动脉事件风险。
一、研究背景&目的
冠状动脉、脑血管和外周血管床中的急性动脉血管事件通常是严重的或致残的,是动脉粥样硬化最可怕的表现。
本研究旨在评估PCSK9抑制剂依洛尤单抗对ASCVD患者各血管区域急性动脉事件的影响。
二、研究方法
FOURIER是一项在 27,564名接受最大耐受他汀类药物治疗,且LDL-C≥70 mg/dL的稳定动脉粥样硬化患者(既往心肌梗死、既往非出血性卒中或有症状的PAD)中进行的PCSK9抑制剂依洛尤单抗对比安慰剂的随机对照试验,中位随访时间为2.2年。下表列出了所有的血管区域的急性动脉事件(表1)。
表 1 所有的血管区域的急性动脉事件

三、研究结果
3.1 依洛尤单抗治疗可显着降低所有的血管床的急性动脉事件发生的风险
研究发现,他汀联用依洛尤单抗可显着降低急性动脉事件发生的风险,包括所有血管床的急性动脉事件和各血管床(包括冠脉事件,脑血管事件和周围血管事件)的急性动脉事件 (图1)。
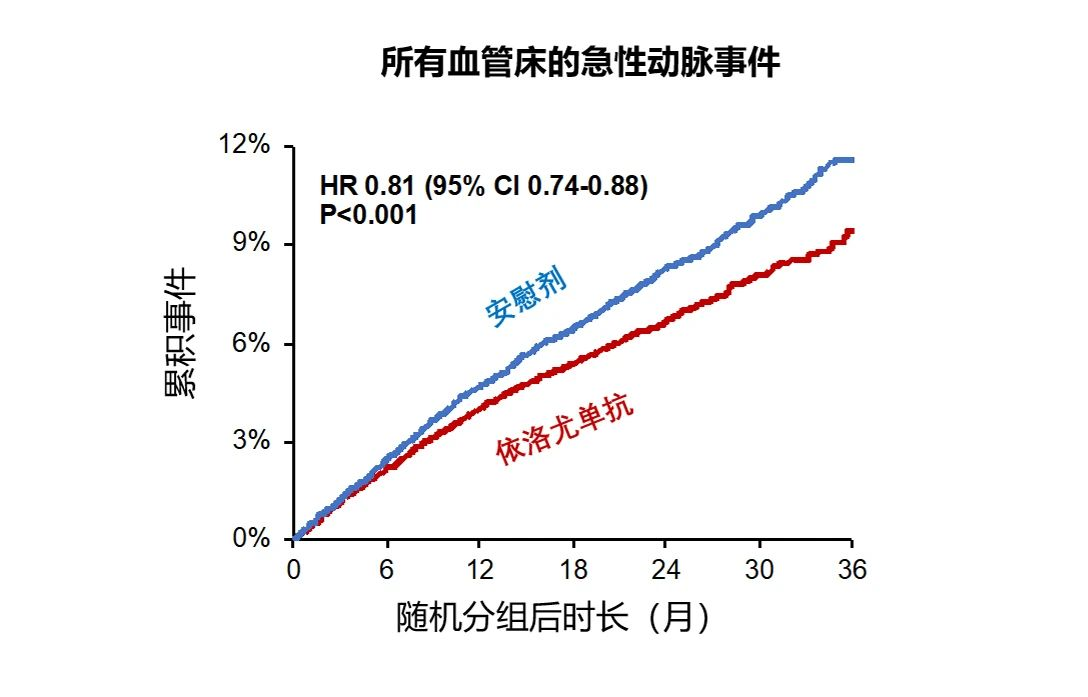
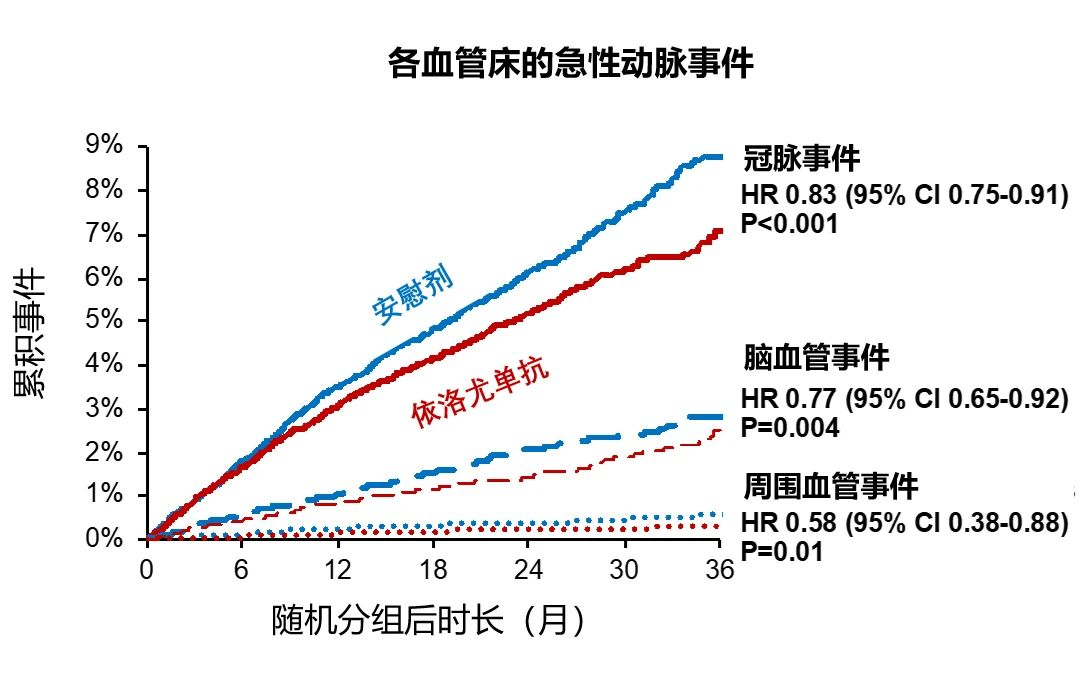
图1 所有的血管床 (上图)和各血管床 (下图)的急性动脉事件发生率
3.2 依洛尤单抗治疗,可显着降低12月内和12月后首次、复发和总急性动脉事件的累积发生率
Landmark分析显示依洛尤单抗治疗12月后即可显着降低累积事件的发生概率,且随着治疗时间的推移,治疗获益更大(图2)。
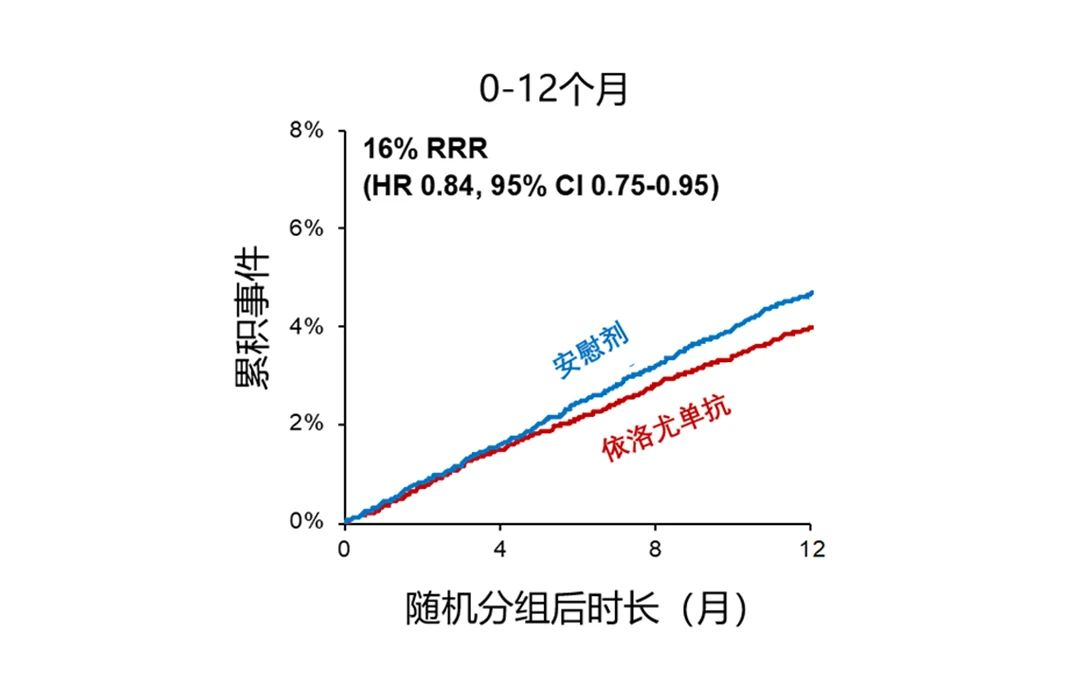
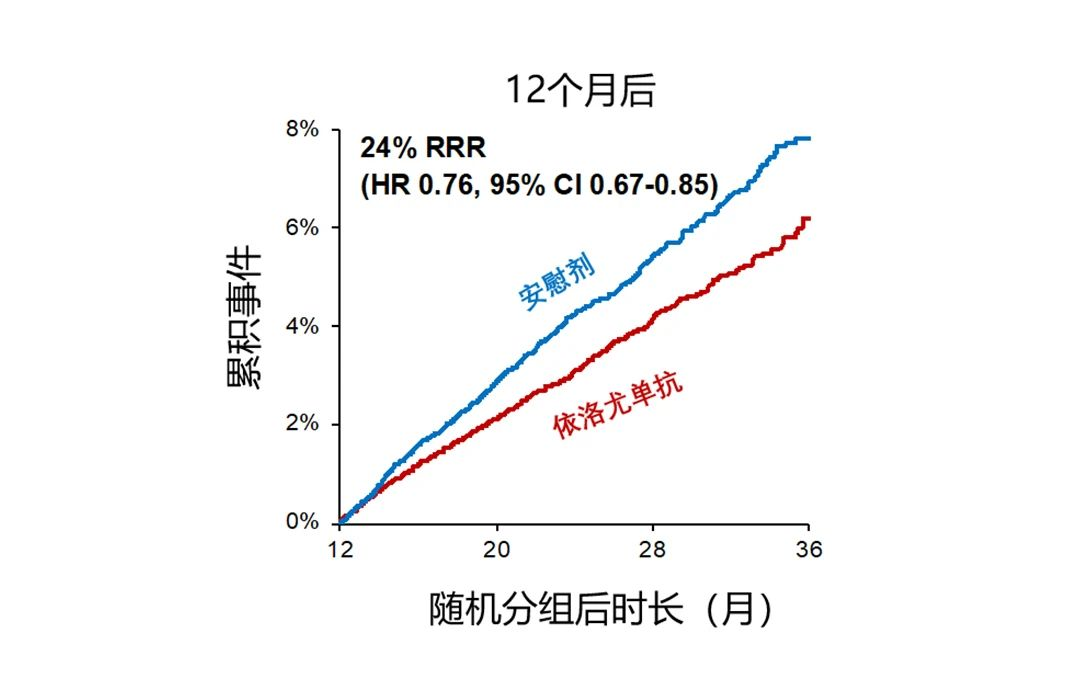
图2 依洛尤单抗疗效的标志性分析
与安慰剂组相比,依洛尤单抗治疗后可以显着降低首次,复发和总急性动脉事件的发生(图3)。
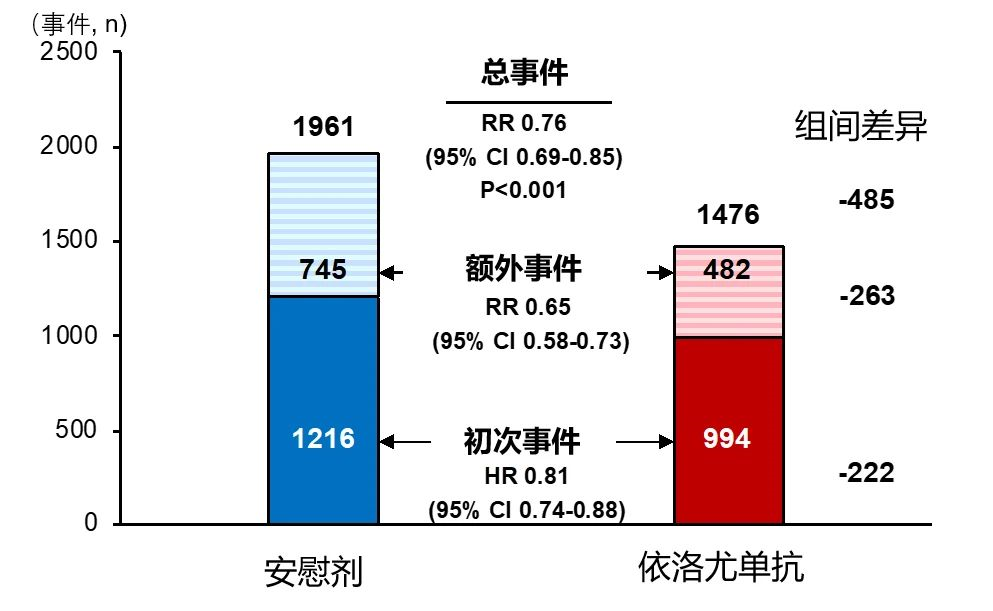
图3 依洛尤单抗对首次、复发和总急性动脉事件影响
四、简评
近期发布的《中国心血管健康与疾病报告2020概要》显示,2018年心血管病死亡仍占我国城乡居民总死亡原因的首位,农村为46.66%,城市为 43.81%。推算我国心血管病现患人数3.30亿,其中脑卒中1300万,冠心病1139 万,下肢动脉疾病4530万。在积极推进零级预防和一级预防的同时,这些不同血管床的ASCVD患者的二级预防是需要我们临床医生关注的焦点,也是我们心血管医生的日常工作重点,而减少甚至避免ASCVD事件再发是ASCVD患者管理的最终目的。FOURIER研究这项最新分析证实了依洛尤单抗治疗可以显着降低各个血管床(心脏、脑和外周动脉)急性动脉事件的发生,进一步夯实了其在ASCVD尤其是极高危/超高危ASCVD患者二级预防中的作用和地位,期待其应用能够为更多ASCVD患者带来全面降低各血管床事件的获益。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#学习#
91
新药新希望……
82
#ASC#
65
#ASCVD#
120