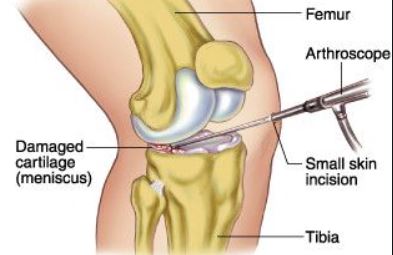
膝半月板损伤普遍发生在体力活动者和普通人群中,年发病率为66-70/10万人。半月板切除术是膝关节骨关节炎的主要风险因素,因此人们努力开发解决方案,尽可能多地保留或恢复半月板。但目前,关节镜下孤立半月板切除术(AM)仍然是最常用的骨科手术之一。
半月板切除术是一种将受损的半月板部分或完全切除的手术。这需要对膝关节进行手术创伤,需要进行术后管理以促进关节功能的正常恢复。在过去的几十年中,许多研究对AM术后的治疗进行了调查。一些研究人员调查了基于家庭的康复计划(HBP),而不是标准的住院和/或门诊监督下的物理治疗(IOP)。
鉴于全球范围内进行的AM手术数量众多,其社会影响和成本,并考虑到HBP与IOP相比可以降低成本,了解基于HBP的AM术后管理的潜力和局限性,对全世界的病人、医生和医疗系统都有很大意义。
为了比较AM术后HBP与IOP的恢复情况,来自瑞士和爱尔兰的骨科专家在PubMed、Web of Science、Cochrane Library和Scopus数据库中进行了系统的文献检索和META分析,相关结果发表在《美国医学会杂志》子刊JAMA Network Open杂志上。
主要结果是Lysholm评分(0-100分,分数越高表示膝关节功能越好),次要结果是主观的国际膝关节文献委员会(IKDC)评分、膝关节伸展和屈曲、大腿围度、水平和垂直跳跃测试,以及PROSPERO注册中显示的恢复工作天数。
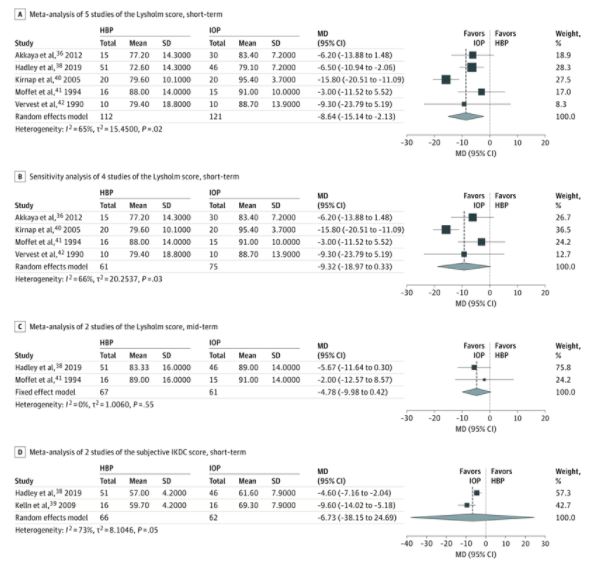
在这项包括434名患者的8项RCT的荟萃分析中,与HBP相比,IOP与Lysholm评分的短期改善有关,2种方法的平均差异为-8.64分(95%CI:-15.14--2.13;P=0.02),但敏感性分析显示没有差异。
HBP(实验组)与IOP(对照组)两组患者报告的结果的森林图
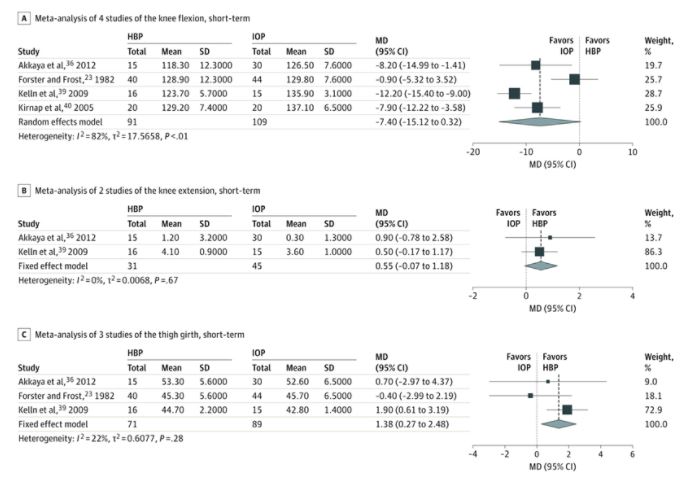
同样,在中期(28-50天)没有发现Lysholm评分有统计学意义的差异,组间平均差异为-4.78分(95%CI,-9.98-0.42;P = .07)。HBP与大腿围的短期改善有关,组间平均差异为1.38cm(95%CI,0.27-2.48cm;P = .01),而IOP与短期垂直跳跃得分的改善有关,组间平均差异为-3.25cm(95%CI,-6.20至-0.29cm;P = .03)。所有其他次要结果都没有发现差异。
对2项研究的元分析没有显示恢复工作时间的组间差异;MD为4.53天(95%CI,-0.39-9.44天;P=0.07)。发现的最大MD是12.6天。
HBP(实验组)与IOP(对照组)两组患者体能结果森林图
在短期和中期随访中,没有发现任何干预措施在身体和功能结果以及工作相关和病人报告的结果方面有优势。但结合家庭康复计划简易可行且符合防疫政策,研究人员认为,在膝关节半月板置换术后,基于家庭的康复计划可能是一种有效的管理方法。
参考文献:
Home-Based vs Supervised Inpatient and/or Outpatient Rehabilitation Following Knee Meniscectomy A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4(5):e2111582. doi:10.1001/jamanetworkopen.2021.11582
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#切除术#
66
#静养#
69
#半月板#
92
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
58