JCO:中国建立术后NSCLC患者的生存预测模型
2015-02-01 MedSci MedSci原创
上述新分期的直接结果是:对于部分病例,根据新分期制定的治疗策略将完全不同于应用旧分期时的策略,而且可能会给这部分患者带来更好的预后。 2015年1月26日,《临床肿瘤学杂志》(J Clin Oncol)在线发表了我国广州医科大学附属第一医院何建行教授团队的一篇文章,详细介绍了一个预测术后非小细胞肺癌(NSCLC)患者生存的模型。 研究详情 通过对中国多中心共6111例术后NSCL
上述新分期的直接结果是:对于部分病例,根据新分期制定的治疗策略将完全不同于应用旧分期时的策略,而且可能会给这部分患者带来更好的预后。
2015年1月26日,《临床肿瘤学杂志》(J Clin Oncol)在线发表了我国广州医科大学附属第一医院何建行教授团队的一篇文章,详细介绍了一个预测术后非小细胞肺癌(NSCLC)患者生存的模型。研究详情
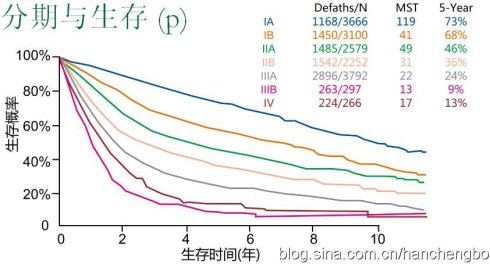
通过对中国多中心共6111例术后NSCLC患者的数据进行分析,研究者确定并整合了与生存相关的预后因素来建立一个预测模型。该模型对来自国际肺癌研究学会(IASLC)数据库单独队列中的2148例患者进行了引导内部验证和外部验证。
结果显示,共有5261例患者纳入分析当中,共6个独立的预后因素进入模型。患者1、3、5年总生存(OS)期的校准曲线概率,在预测模型与实际观察中达 到高度一致。预测模型比美国癌症联合委员会第7版的TNM分期系统的一致性指数(C-index)更高(主要研究队列中,0.71对 0.68,P<0.01;国际肺癌研究学会队列中,0.67对0.64,P=0.06)。
结论
研究者建立和验证了一项新的模型,能够有效预测术后NSCLC患者的生存。该预测模型的使用或可帮助临床医生制定治疗决策和设计临床试验。
原始出处:
Liang W, Zhang L, Jiang G, Wang Q, Liu L, Liu D, Wang Z, Zhu Z, Deng Q, Xiong X, Shao W, Shi X, He J.Development and Validation of a Nomogram for Predicting Survival in Patients With Resected Non-Small-Cell Lung Cancer.J Clin Oncol. 2015 Jan 26. pii: JCO.2014.56.6661
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCO#
66
#SCLC患者#
60
中国学者
135
#预测模型#
64
#NSCLC患者#
0