Lancet Oncol:杜瓦鲁单抗联合曲美木单抗治疗晚期转移性肉瘤
2022-08-11 MedSci原创 MedSci原创
对于晚期或转移性肉瘤患者,杜瓦鲁单抗和曲美木单抗的联合方案是一种有效的治疗策略。
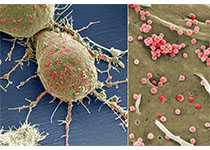
转移性肉瘤患者几乎没有标准的治疗选择。该研究旨在评估PD-L1药物杜瓦鲁单抗和抗CTLA-4药物曲美木单抗在多种肉瘤亚型中的疗效、安全性和肿瘤微环境的变化。
这是一项单中心的2期试验,招募了年满18岁、既往至少接受过一次系统治疗的、ECOG表现状态0-1分的晚期或转移性肉瘤患者,予以静脉杜瓦鲁单抗(1500 mg)和曲美木单抗(75 mg)治疗4个疗程,继以杜瓦鲁单抗单药维持(1次/4周),到12个月。主要终点是12周时的无进展生存率。
无进展生存率
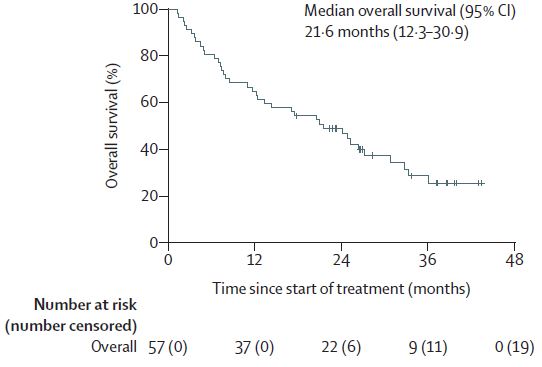
2016年8月17日至2018年4月9日期间,共招募了62位患者,其中57位(92%)接受了研究治疗被纳入意向治疗人群。截止2020年4月30日,中位随访了37.2个月(范围 1.8-10.1),12周时的无进展生存率是49%(95% CI 36-61)。中位无进展生存期是2.8个月,12个月无进展生存率是28%,24个月无进展生存率是15%。中位总生存期是21.6个月。12个月总生存率是65%,24个月总生存率是49%。
总生存率
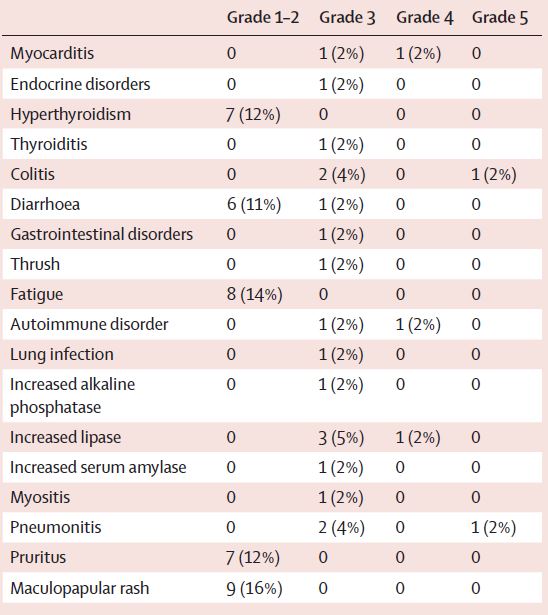
共报告了21例3-4级的治疗相关不良反应,最常见的有脂肪酶升高(7%)、结肠炎(5%)和肺炎(5%)。9位(16%)患者经历了治疗相关的严重不良反应事件。1位患者发生了5级的肺炎和结肠炎。
治疗相关不良反应
综上,对于晚期或转移性肉瘤患者,杜瓦鲁单抗和曲美木单抗的联合方案是一种有效的治疗策略,值得进一步开展相关试验进行评估。
原始出处:
Neeta Somaiah, et al. Durvalumab plus tremelimumab in advanced or metastatic soft tissue and bone sarcomas: a single-centre phase 2 trial. The Lancet Oncology. August 04, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
0
#Oncol#
81
#转移性#
127
lancet上果然牛,感谢梅斯更新及时
84