JAMA Surg:NSCLC患者手术治疗中先处理动脉还是静脉?
2019-05-11 不详 网络
在手术期间首先结扎出血静脉还是动脉,更能减少非小细胞肺癌患者肿瘤细胞的传播吗?因此,本研究旨在比较的术中不同血管离断顺序对NSCLC患者肿瘤细胞扩散及生存状况的影响。此为一项多中心随机临床试验,于2016年12月至2018年3月在华西医院、大坪医院、四川肿瘤医院接受胸腔镜肺叶切除术的NSCLC患者中进行。为了进一步比较两种手术的生存结果,我们使用相同的纳入标准对中国西部肺癌数据库(2005-201
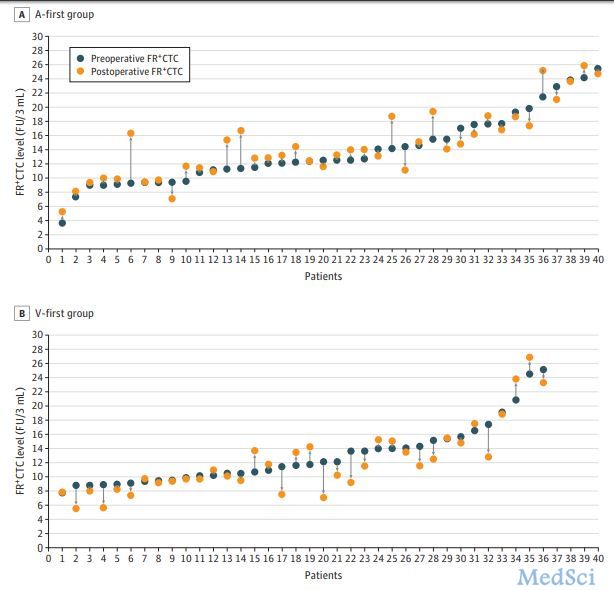
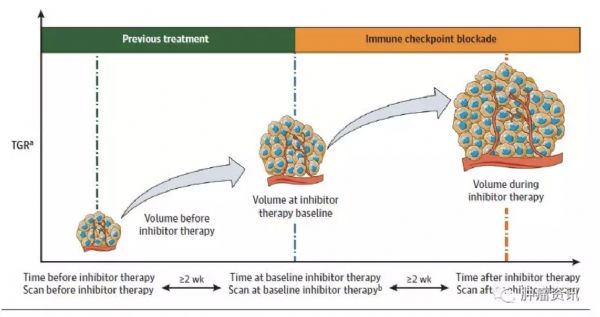
在手术期间首先结扎出血静脉还是动脉,更能减少非小细胞肺癌患者肿瘤细胞的传播吗?因此,本研究旨在比较的术中不同血管离断顺序对NSCLC患者肿瘤细胞扩散及生存状况的影响。此为一项多中心随机临床试验,于2016年12月至2018年3月在华西医院、大坪医院、四川肿瘤医院接受胸腔镜肺叶切除术的NSCLC患者中进行。为了进一步比较两种手术的生存结果,我们使用相同的纳入标准对中国西部肺癌数据库(2005-2017)进行了回顾性分析。先离断静脉与先离断动脉对比。术后叶酸受体阳性循环肿瘤细胞(FR+CTCs)和5年总体无病生存、肺癌特异性生存率的变化。共随机抽取86人;22例(25.6%)年龄小于60岁,46例(74.4%)年龄大于60岁。最后纳入其中78例患者进行分析。动脉先断组的40名患者中有26例(65.0%)出现FR+CTC增多,而静脉先断组的38名患者中有12例(31.6%)增多(中位变化为0.73 [四分位间距(IQR), - 0.86 - 1.58] / 3mL FU 相比 - 0.50 [IQR, - 2.53 - 0.79] / 3mL FU;P = 0.006)。多因素分析证实先断动
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SCLC患者#
25
#静脉#
38
#手术治疗#
29
#NSCLC患者#
30
谢谢分享学习
69
研究不在于大小,关键在于对临床的贡献,这个研究非常有意义,值得学习。
64
非常有价值
60
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
46