主治考试知识考点-产后大出血典型病例1例
2017-05-24 MedSci MedSci原创
“产后大出血”是指胎儿娩出后,经阴道生产的产妇出血超过500毫升,或经剖腹生产的产妇出血超过1000毫升。当产妇失血量达至一定程度,即有可能发生生命迹象不稳定、广泛性凝血功能低下,甚至休克及死亡。产后出血是执业医师、主治医师考试中常见的考点,梅斯小编整理了产后出血典型病例1例,供大家参考!主诉:患者,33岁,G2P1。因产后阴道大量出血8小时由外院转入。[病史概要]该产妇因孕41周于 4月2日住当
【主诉】
【病史概要】
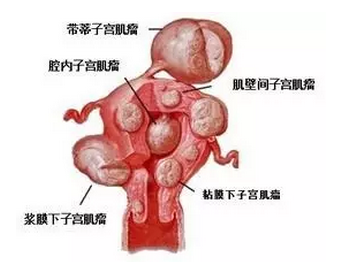
该产妇因孕41周于 4月2日住当地医院待产,并于入院当天以延期妊娠予以0.5%浓度缩宫素静滴计划分娩。静滴缩宫素2天无效,于4月4日上午再次以1%浓度缩宫素静滴,下午10时临产,4月5号0时30分宫口开全,0时50分顺产分娩一男婴,体重3600g,胎盘自娩完整,会阴II度裂伤,产后即时阴道出血400ml。检查发现宫颈3点、9点处和阴道左侧壁裂伤,随即缝合止血,并予米索前列醇400ug 和缩宫素20U促宫缩治疗,出血未止。至4月5日上午4时30分累计出血达1600ml。在静脉输液、输血、促宫缩治疗的同时,再次行阴道、宫颈裂伤创口缝合止血,并做清宫术,未见胎盘胎膜残留,事后曾一度出血减少。但观察1小时后,阴道出血又逐渐增加,至4月5日上午8时又出血700ml,心率120次/分,血压90/60 mmHg,急送本院。既往体健。
【体格检查】
【辅助检查】
更多此病例详情请点击:考点回顾-产后大出血病例1例
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#产后大出血#
110
学习了谢谢分享
128
继续学习中谢谢分享
127
#大出血#
114
#考试#
101