Cell Res:曹雪涛院士亮点推荐了一项癌症新成果
2015-12-29 佚名 生物通
12月25日,曹雪涛院士在nature子刊Cell Research杂志上发表了一篇题为“Organotropic metastasis: role of tumor exosomes”的文章,为我们亮点推荐了近期发布在《自然》(Nature)杂志上的一项癌症新成果。在这篇文章中,来自美国Meyer癌症中心的研究人员证实表达独特整合素(integrins)的肿瘤外泌体(exosome)可通过它们的
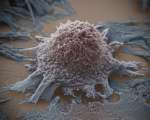
12月25日,曹雪涛院士在nature子刊Cell Research杂志上发表了一篇题为“Organotropic metastasis: role of tumor exosomes”的文章,为我们亮点推荐了近期发布在《自然》(Nature)杂志上的一项癌症新成果。在这篇文章中,来自美国Meyer癌症中心的研究人员证实表达独特整合素(integrins)的肿瘤外泌体(exosome)可通过它们的整合素介导与器官特异性定居细胞融合来准备转移前微环境,由此决定了器官性特异性癌症转移。
肿瘤转移是肿瘤恶性进展至关重要的一步,与大多数癌症治疗失败有关。癌症转移的一个显特点就是,在一些细胞及分子程序的控制下,某些类型的癌细胞优先定植及转移至特异器官处。当前许多的研究都主要将焦点放在鉴别这种器官特异性癌症转移的细胞内在决定因素上,包括癌细胞表达的基因和趋化因子受体。一些粘附及胞外基质分子,如整合素、细胞粘合素(tenascin)和骨膜蛋白(periostin)也被证实促进了转移癌细胞定植。
2005年,Lyden博士和同事们提出了一个叫做“转移前微环境”的术语来描述原发肿瘤可通过招募骨髓源性细胞到远端器官处,建立支持性的转移微环境来促进自身转移。此外,也有研究报道肿瘤源性可溶因子如赖氨酰氧化酶(lysyl oxidase)通过在某些位点形成转移前微环境诱导器官特异性转移。但目前对于器官特异性癌症转移的机制仍然不是很清楚。
近年来,有研究证实肿瘤源性外泌体促进了癌症进展。外泌体是包含着一些功能生物分子(包括蛋白质、RNA、DNA和脂质)的有膜结构的小囊泡,它们可以将这些生物分子水平传递给接受细胞。例如,脑星形胶质细胞源性外泌体可以通过将靶向PTEN的microRNA-19a传递给这些癌细胞来促进脑转移癌细胞生长。尽管如此,对于肿瘤外泌体上的一些分子是否决定了器官特异性转移仍是个待解的问题。
在这篇Nature文章中Lyden和同事们给出了答案,证实肿瘤外泌体整合素可通过与器官特异性定居细胞融合来建立转移前微环境,决定器官特异性癌症转移。他们从已知主要转移至肺、肝和脑器官处的小鼠和人类乳腺癌及胰腺癌细胞系中分离出了外泌体,证实它们优先与预计目的地的定居细胞,即肺成纤维细胞与上皮细胞、肝枯否细胞(Kupffer cell)和脑内皮细胞融合。
器官特异性细胞摄取肿瘤源性的外泌体从而准备好转移前微环境。研究人员证实用来自肺转移倾向肿瘤的外泌体进行处理,可以让有骨转移倾向的肿瘤细胞转移重定向。外泌体蛋白质组揭示出了不同的整合素表达模式:外泌体整合素α6β4和α6β1与肺转移相关,外泌体整合素αvβ5与肝转移相关。靶向整合素α6β4和αvβ5可以减少外泌体摄取,并分别抑制肺转移和肝转移。Lyden和同事们还证实定居细胞摄取外泌体整合素激活了Src磷酸化和促炎症S100基因表达。他们的临床数据表明可以利用外泌体整合素来预测器官特异性癌转移。
在文章的最后,曹雪涛院士指出Lyden和同事们的这项研究扩展了我们对于器官特异性癌症转移一机制的认识,也突出强调了外泌体在促进肿瘤转移中至关重要的作用。
原始出处:
A recent paper in Nature shows that tumor exosomes expressing unique integrins can determine organotropic metastasis by preparing pre-metastatic niche through their integrins-mediated fusion with and fertilization of organ-specific resident cells.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新成果#
91
#Cell#
69
#CEL#
80
肿瘤研究新方向
135
#曹雪涛#
71
这才是高质量的研究!
159
看不懂
154
希望有更多的依据支持
154
赞一个
170
牛
106