Cell Death Dis:广州生物院发现基因治疗佐剂引发神经退化
2018-09-27 佚名 广州生物院
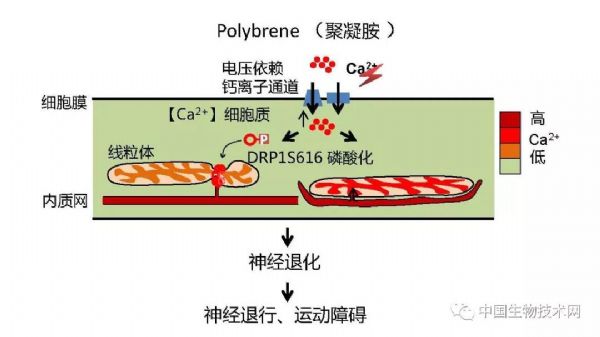
该研究发现,Polybrene作为广泛使用的基因治疗和感染的佐剂,在低剂量下引发神经退化:小鼠的体内实验表现出运动障碍伴随脑内神经死亡和胶质增生,而在人神经元中诱发浓度依赖性轴突串珠化和碎片化。这一神经毒性的机制是钙离子内流双向调控细胞器重塑:线粒体断裂,内质网片段化并和线粒体耦合,而启动神经退化。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
63
#Cell#
62
#Dis#
74
#Death#
54