Front Neurosci:一石二鸟!咖啡竟可防帕金森和老年痴呆!
2018-11-09 Michael,Zoe 转化医学网
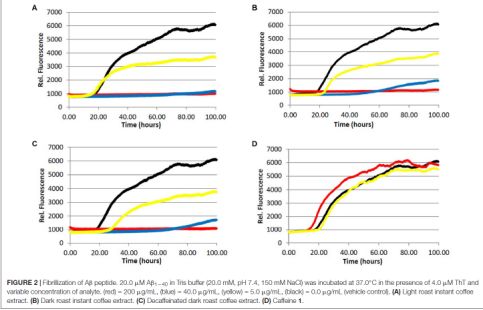
。近几年的研究发现,咖啡这种神奇的饮品对于预防各种疾病都有很好的作用,从预防心脏病到降低抑郁的发生,都能看到研究咖啡具有保护作用的文章。最新的研究发现,长喝咖啡竟然能够预防老年后帕金森的发病,这对众多咖啡依赖者来说又多了一个好事,这项研究的最新进展发表于近期的《Frontiers in Neuroscience》杂志。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ROS#
116
123
163
研究的好
115
好
139
这么啊?
0
老年人痴呆何药可用??
0