J Thorac Oncol:Lorlatinib(劳拉替尼)治疗ALK+ NSCLC患者进展后继续使用仍然有效
2022-01-18 yd2015 MedSci原创
近期,在Journal of Thoracic Oncology杂志上发表了一项研究成果,主要是回顾性分析II期临床研究(NCT01970865)的数据,评估Lorlatinib(劳拉替尼)治疗的AL
近期,在Journal of Thoracic Oncology杂志上发表了一项研究成果,主要是回顾性分析II期临床研究(NCT01970865)的数据,评估Lorlatinib(劳拉替尼)治疗的ALK+ NSCLC患者进展后继续使用Lorlatinib的疗效。
回顾性分析正在进行的II期试验(NCT01970865)中进展患者(LBPD)后继续服用Lorlatinib的临床益处。既往仅使用克唑替尼作为ALK TKI的患者为A组(n = 28);既往使用过≧1种二代ALK TKIs患者为B组(n = 74)。LBPD定义为Lorlatinib治疗≧3周后研究者评估病情进展。只有Lorlatinib治疗获得完全或部分缓解或病情稳定的患者进展后才被纳入。
A和B组的中位随访时间分别为 35.2和34.2个月。A组患者中,LBPD和非LBPD患者初始Lorlatinib治疗的ORR分别为71.4%和71.4%;颅内ORR分别为66.7%和37.5%。B组患者中,LBPD和非LBPD患者初始Lorlatinib治疗的ORR分别为46.4%和22.2%;颅内ORR分别为39.5% 和25.0%。
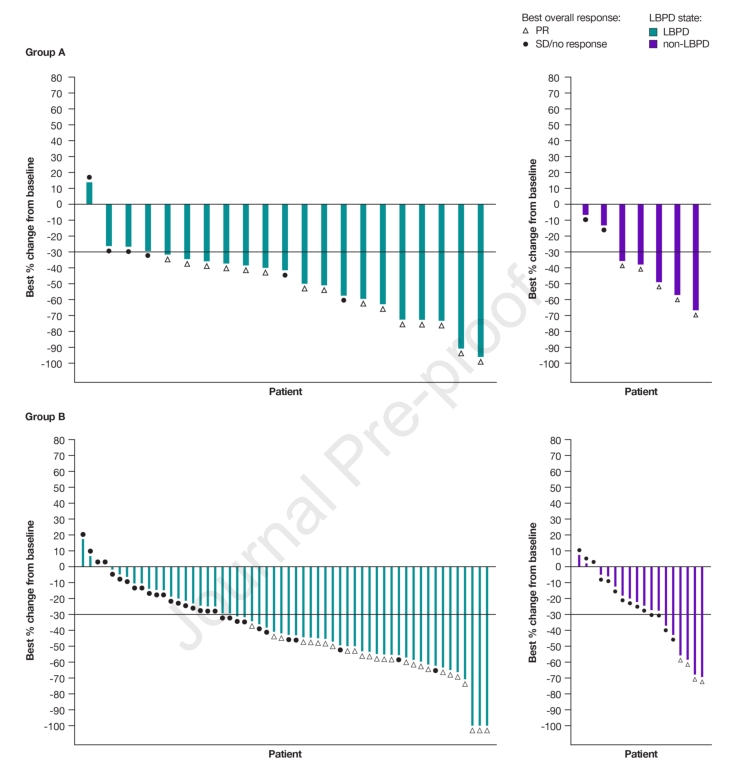
与非LBPD患者相比,LBPD患者的颅外进展更少(A组:71.4% vs 100.0%;B组:67.9%对94.4%)。此外,在A组患者中,LBPD患者比非LBPD患者有更多的目标病变进展(76.2% vs 42.9%),新病变更少(28.6% vs 57.1%)。在B组患者中,LBPD和非LBPD患者均有广泛的进展,许多患者有靶病变进展(41.1% vs 61.1%)和新病变(42.9%vs 44.4%)。
大约四分之一的非LBPD患者没有接受任何后续治疗。在接受后续治疗的患者中,很多人接受了不同的ALK TKI治疗(A组71.4%,B组55.6%)。A组LBPD患者接受放疗的比例为9.5%,B组LBPD患者接受放疗的比例为8.9%。
LBPD患者的总中位治疗时间为32.4个月(A组)和16.4个月(B组),而非LBPD患者的总中位治疗时间为12.5个月(A组)和7.7个月(B组)。A和B组LBPD患者进展后治疗中位时间分别为 11.8和5.7个月。
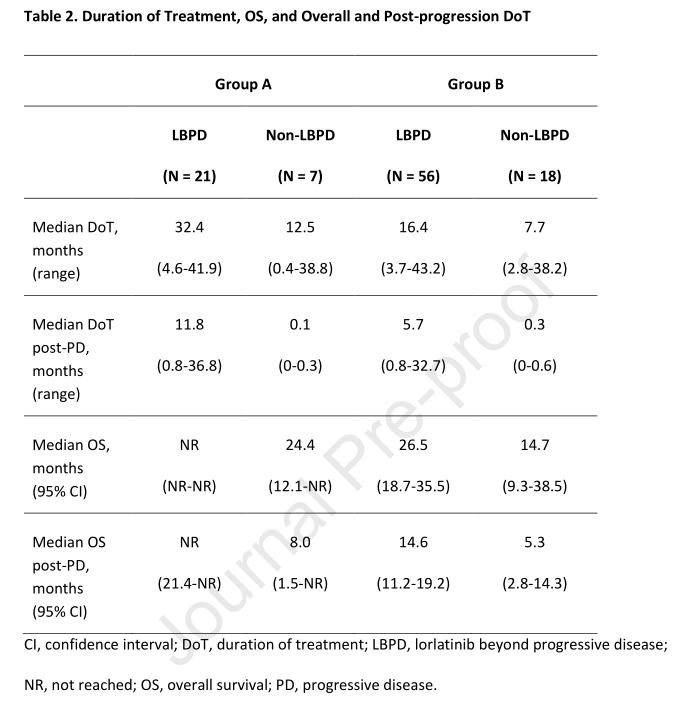
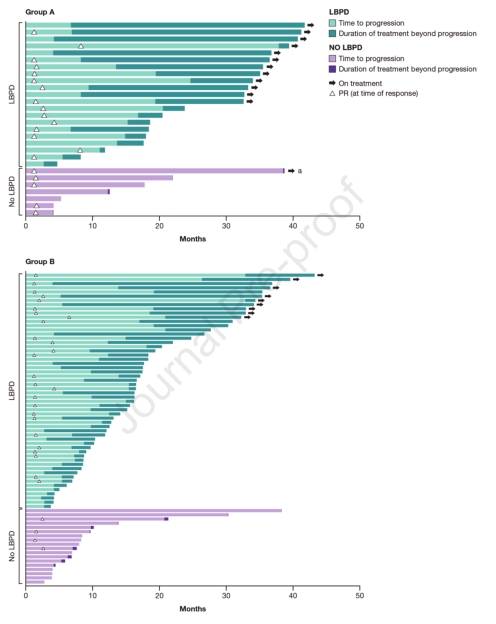
A组患者中,LBPD患者总中位总生存期(OS)没有达到(NR),而非LBPD患者的总中位总生存期为24.4个月(95%CI 12.1-NR);B组患者中,LBPD患者的总中位OS为26.5个月(95% CI 18.7-35.5),而非LBPD患者为14.7个月(95% CI 9.3-38.5)。
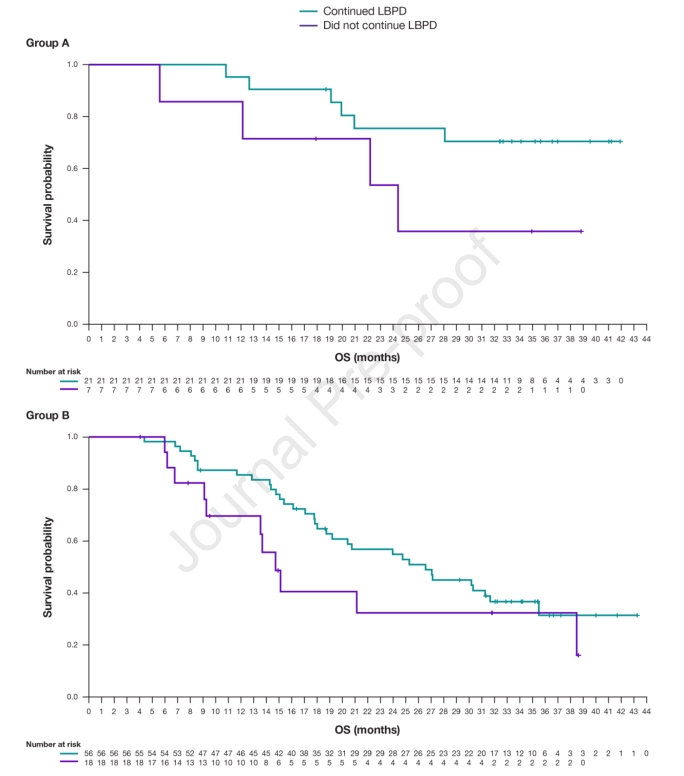
A组患者中,LBPD患者进展后的中位OS未达到,非LBPD患者进展后中位OS为8.0个月(95% CI 1.5-NR);B组患者中,LBPD患者进展后的中位OS 为14.6个月(95% CI 11.2-19.2),非LBPD患者进展后中位OS为5.3 个月(95% CI 2.8-14.3)。
综上,研究表明,Lorlatinib(劳拉替尼)治疗ALK+ NSCLC患者进展后继续使用是一种可选择策略。
原始出处:
Ou SI, Solomon BJ, Shaw AT, Gadgeel SM, Besse B, Soo RA, Abbattista A, Toffalorio F, Wiltshire R, Bearz A. Continuation of Lorlatinib in ALK-positive NSCLC Beyond Progressive Disease. J Thorac Oncol. 2022 Jan 10:S1556-0864(21)03417-1. doi: 10.1016/j.jtho.2021.12.011. Epub ahead of print. PMID: 35026476.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SCLC患者#
134
#ALK+#
83
#Oncol#
64
#THORAC#
59
#NSCLC患者#
74