European Radiology:用这个MRI序列,对软组织肉瘤进行病理级放大!
2022-07-01 shaosai MedSci原创
Ki-67是一种仅在细胞增殖期间表达的核蛋白,与肿瘤的侵袭性有关,已被广泛用于预测乳腺癌、肺癌、膀胱癌、鼻咽癌和星形细胞瘤患者的预后和治疗后反应,也是STS生存的一个重要的独立预测因素。
众所周知,软组织肉瘤(STS)是一个异质性肿瘤,占所有恶性肿瘤的不到1%,但死亡率很高。Ki-67是一种仅在细胞增殖期间表达的核蛋白,与肿瘤的侵袭性有关,已被广泛用于预测乳腺癌、肺癌、膀胱癌、鼻咽癌和星形细胞瘤患者的预后和治疗后反应,也是STS生存的一个重要的独立预测因素。核心针头活检目前用于STS的术前诊断和评估,但准确性可能会受到肿瘤异质性的影响,从而导致不恰当的治疗和不良的临床预后。因此,迫切需要非侵入性的检查指标进行Ki67 LI的评估。

随着功能性磁共振成像(MRI)的发展,非侵入性的成像方法已用来评估STS的生化、结构和代谢特征。由单指数扩散加权成像(DWI)模型计算出的表观扩散系数(ADC)值是预测STS中Ki-67 LI的潜在指标。然而,ADC值不仅受水分子运动的影响,而且还受微血管灌注的影响。IVIM双指数模型可以区分体内灌注和扩散的成像效果。DKI可以通过使用更高的b值来评估肿瘤的异质性和复杂性。
近日,发表在European Radiology杂志的一项研究探讨了IVIM和DKI作为评估STSKi-67表达的非侵入性影像学指标的诊断性能。
41名STS患者接受了3.0MRI的IVIM和DKI成像。由两名独立观察员对Ki-67低表达组和高表达组的标准表观扩散系数(ADC)、真实扩散系数(D)、伪扩散系数(D*)、灌注分数(f)、平均峰度(MK)和平均扩散率(MD)进行了比较。使用了一种新的方法来确保组织学切片和磁共振成像切片的地形相关性。接受者操作特征(ROC)、类内相关系数(ICC)和Spearman等级相关进行了统计分析。
与低表达组相比,高表达组的标准ADC、D和MD值较低,MK值较高。D∗和f值没有发现明显差异。区分低表达组和高表达组时,标准ADC、D、MD和MK的曲线下面积分别为0.736、0.745、0.848和0.894。MK与Ki-67 LI呈正相关(r = 0.809,p < 0.001)。标准ADC、D和MD与Ki-67 LI呈负相关(r = -0.541、-0.556、-0.702,分别为p < 0.001)。
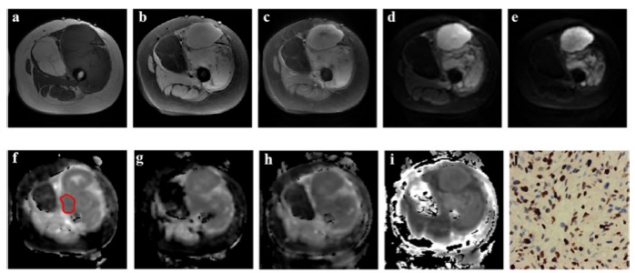
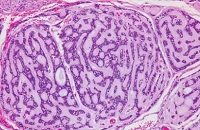
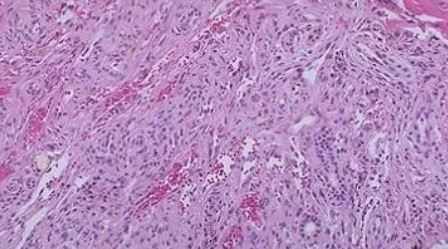
图 一位67岁患有左大腿未分化脂肪肉瘤患者的图像。 a T1加权图像显示一个不规则的稍高信号肿块。b T1脂肪抑制序列显示高信号区域的信号减弱。c 病变的实性部分在注射钆基造影剂后显示轻微的异质性增强,有小块的瘤周强化。 d, e 病变的实性体部分在IVIM(b=100s/mm2)图像上显示高信号,在DKI(b=2000s/mm2)图像上信号强度范围下降。标准ADC(f)、D(g)、MD(h)和MK(i)值分别为1.28×10-3 mm2/s、0.93×10-3 mm2/s、1.01×1010-3 mm2/s和0.82。 j Ki-67 LI为40%,该病变被归入高表达组
本研究发现,IVIM和DKI参数能准确评估STS的Ki-67表达,这有助于肿瘤分级,为进一步的治疗计划提供信息并预测STS的临床预后。
原文出处:
Kai Zhang,Yue Dai,Yajie Liu,et al.Soft tissue sarcoma: IVIM and DKI parameters correlate with Ki-67 labeling index on direct comparison of MRI and histopathological slices.DOI:10.1007/s00330-022-08646-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
60
#MRI序列#
60
#软组织肉瘤#
100
#软组织#
53