JAMA Intern Med:请注意!抗胆碱能药物可能导致阿尔兹海默症的到来
2019-06-28 佚名 生物探索
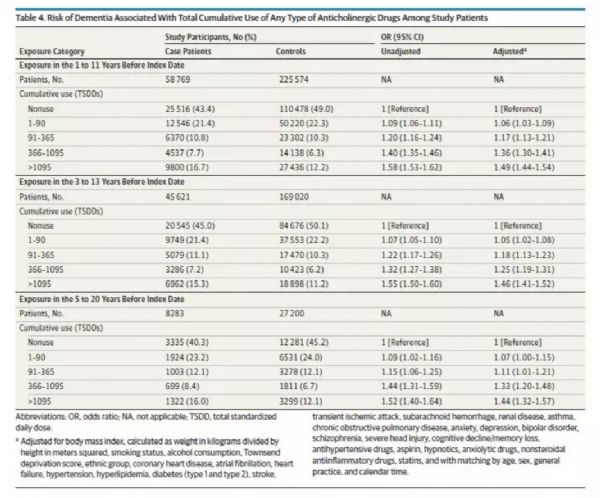
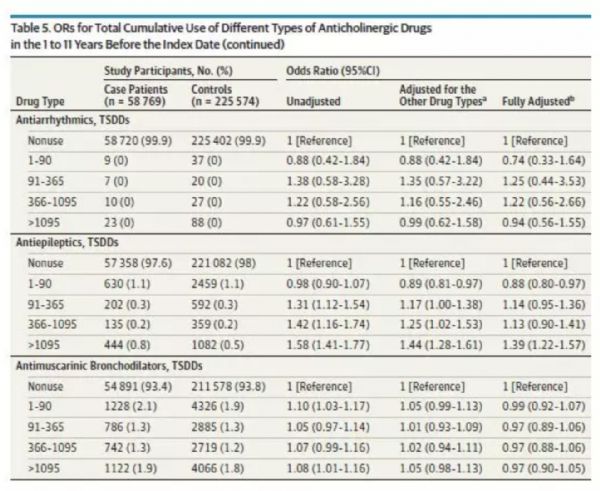
让人惊喜地是,最近发表在《JAMA Internal Medicine》的一篇论文报告了另一个可能的因素:抗胆碱能药物可能会导致阿尔兹海默症的患病风险明显增加。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










谢谢分享
30
#阿尔兹海默#
34
#胆碱#
37
#抗胆碱能药物#
40
#Med#
44
学习了,谢谢分享
0
好
73