J Thorac Oncol:不可切除III期NSCLC放化疗后无进展患者德瓦鲁单抗(durvalumab)维持治疗4年生存分析结果:来自PACIFIC结果更新
2021-05-12 yd2015 MedSci原创
不可切除III期NSCLC放化疗后无进展患者德瓦鲁单抗(durvalumab)维持治疗可获得持续的PFS和OS获益。德瓦鲁单抗维持治疗4年OS和PFS率分别为49.6% 和35.3%,而对照组为36.
不可切除III期NSCLC的标准治疗为以铂类为基础的同步放化疗。但是没有研究表明治疗结束后继续使用药物或其他治疗可使生存获益。直到PACIFIC研究问世,才改写了这一标准治疗。今年J Thorac Oncol杂志更新了4年生存数据。
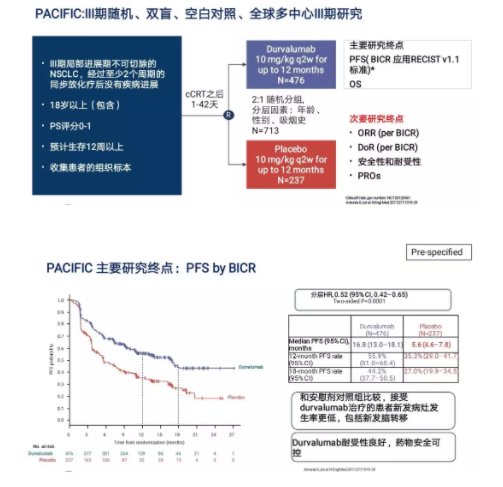
PACIFIC研究是一项随机、双盲、全球的III期临床试验,主要评估不可切除III期NSCLC放化疗后无进展患者德瓦鲁单抗(durvalumab)维持治疗的疗效和安全性。德瓦鲁单抗是一种PDL1抑制剂。患者放化疗结束无进展者随机2:1分配到德瓦鲁单抗组和安慰剂组。德瓦鲁单抗组剂量为10 mg/Kg/2W,共12个月。对年龄、性别、吸烟史等进行分层分析。主要研究终点为无进展生存期(PFS)和总生存期(OS),次要终点为12个月,18个月的PFS率,客观缓解率(ORR),持续缓解时间(DOR)和安全性等。
该研究共713例患者进行随机化,但是只有709例患者接受后续治疗,其中德瓦鲁单抗组473例,安慰剂组为 236例。2017年NEJM杂志首次公布研究数据1。研究数据表明,两组中位PFS为 16.8个月和 5.6个月(HR=0.52; 95% CI: 0.42–0.65; p < 0.0001);12个月的PFS率为55.9% 和 35.3%;18个月的PFS为44.2% 和27.0%. 两组的ORR为 28.4% vs. 16.0% (P<0.001);两组18个月的DOR为 72.8% 和 46.8%; 两组死亡或远处转移的中位时间为23.2个月和14.6个月(P < 0.001); 两组3级或4个不良事件发生为29.9%和 26.1%; 最常见的3级不良事件4例为肺炎(分别为4.4%和3.8%)。两组分别有15.4%和9.8%的患者因严重不良事件停止治疗。
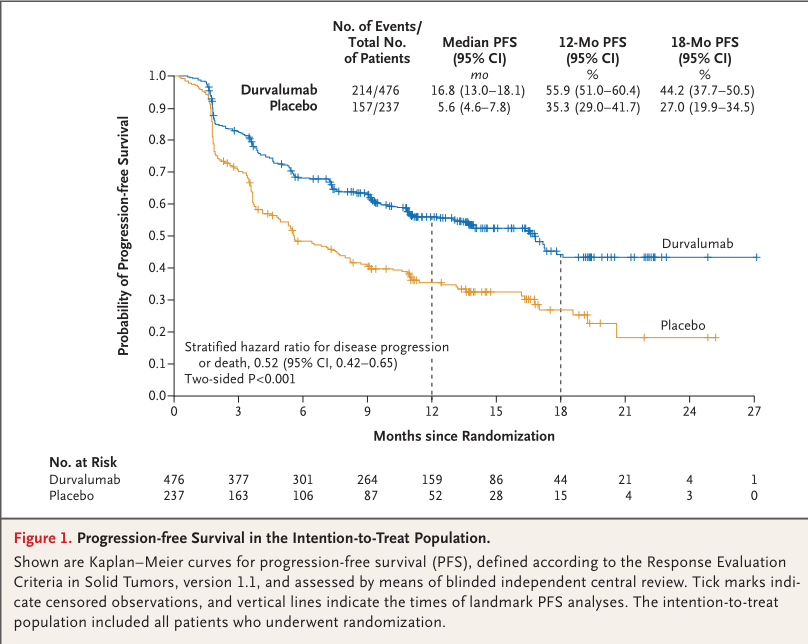
首次报道的两组PFS
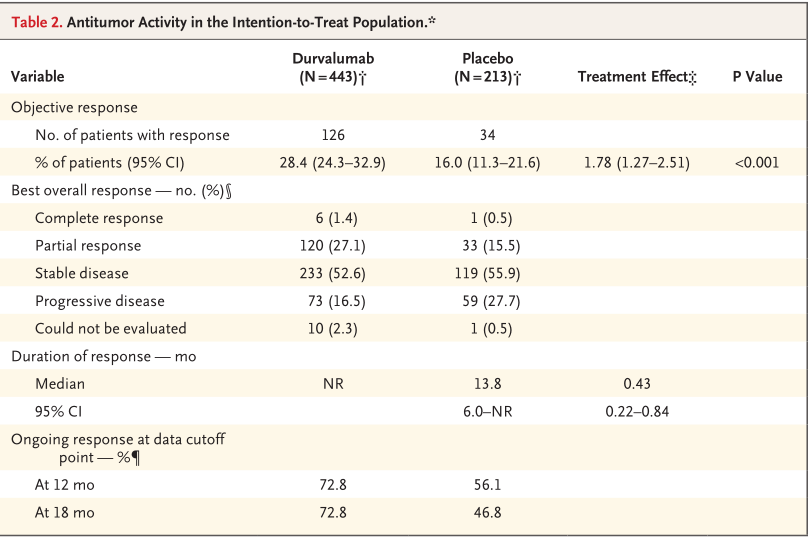
首次报报道的临床获益
2018年NEJM杂志更新研究数据2。截止2018年3月22日,中位随访时间为25.2个月。两组24个月OS为66.3%和55.6% (HR=0.68; 99.73% CI, 0.47 to 0.997; P = 0.0025);两组中位缓解持续时间为17.2和 5.6个月 (HR=0.51;95% CI, 0.41 to 0.63);两组死亡或远处转移的中位时间为28.3个月和16.2个月(HR=0.53; 95% CI, 0.41 to 0.68);两组3级或4个不良事件发生为30.5%和 26.1%;两组分别有15.4%和9.8%的患者因严重不良事件停止治疗。

2年PFS
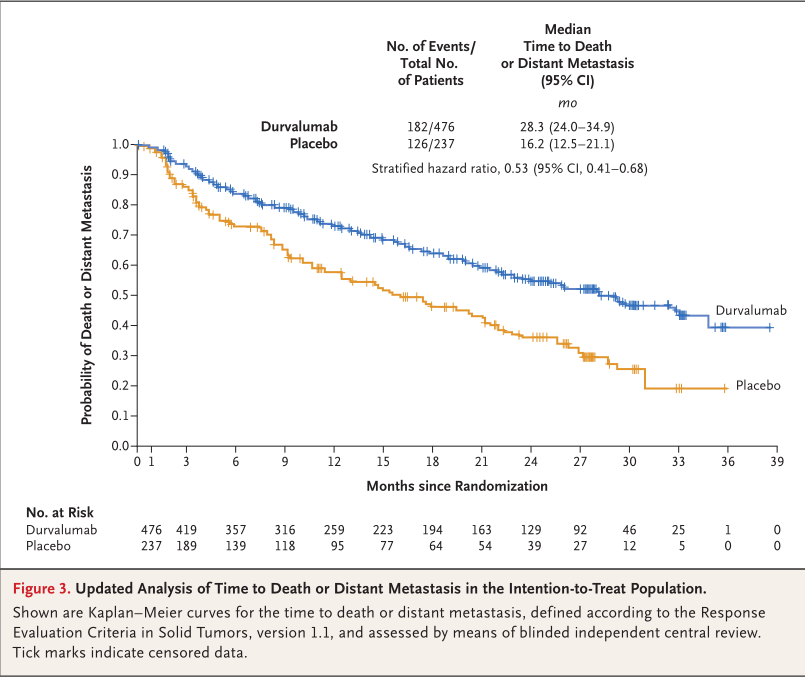
两组的死亡或转移中位时间
2020年J Thorac Oncol杂志更新了3年生存数据3。截止2019年1月31日,共48.2%的患者死亡,其中德瓦鲁单抗组有44.1%患者死亡,而安慰剂组有56.5%患者死亡。中位持续随访时间为33.3个月。两组中位OS为未达到和29.1个月(HR = 0.69,95% CI: 0.55– 0.86);两组的12, 24和36个月OS 率 分别为83.1%和74.6%, 66.3% 和55.3%, 以及57.0% 和43.5%。次要终点结果跟以后报道一致。
.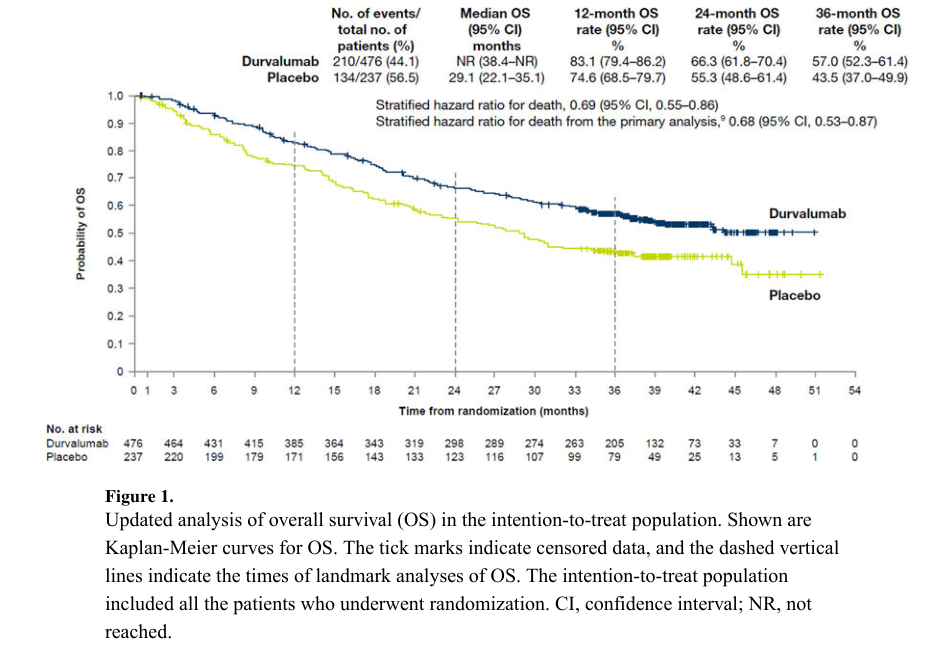
更新两组3年的OS率
今年J Thorac Oncol杂志更新了4年生存数据4。截止2020年3月20日,中位随访34.2个月,两组中位OS为47.5 和29.1 个月(0.71 (95% CI: 0.57–0.88));两组4年的OS率为49.6% 和 36.3%; PFS率为35.3% 和 19.5%。
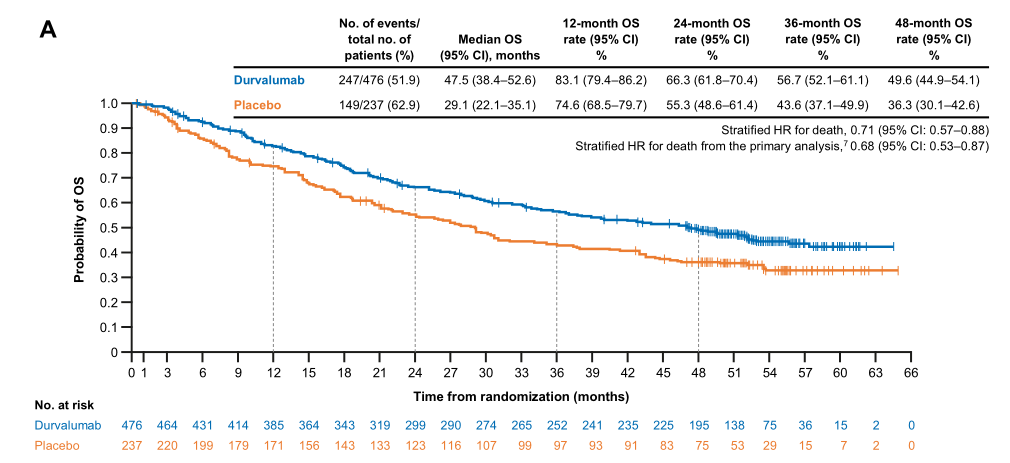
更新的两组两组4年OS率
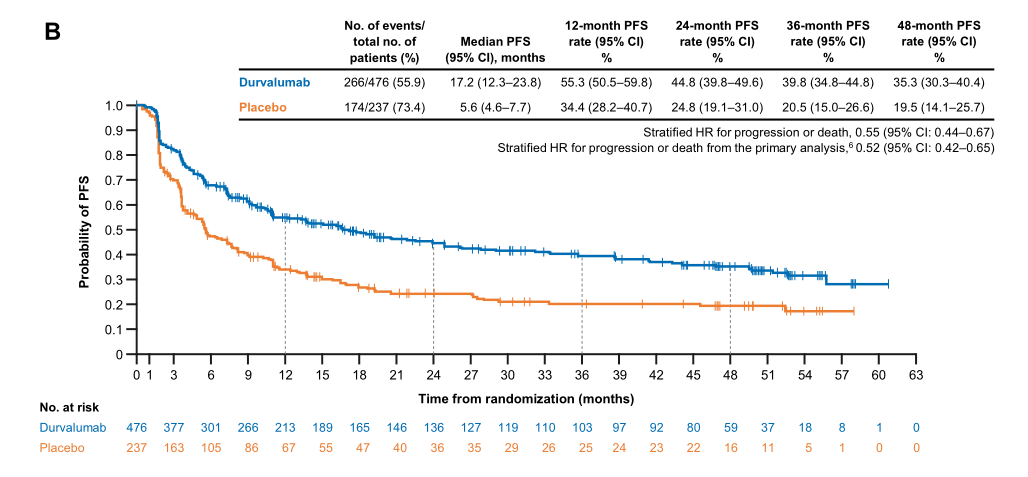
更新的两组4年PFS率
综上,不可切除III期NSCLC放化疗后无进展患者德瓦鲁单抗(durvalumab)维持治疗可获得持续的PFS和OS获益。
原始出处:
1. Scott J Antonia , Augusto Villegas, Davey Daniel, et al. Durvalumab after Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. N Engl J Med. 2017 Nov 16;377(20):1919-1929. doi: 10.1056/NEJMoa1709937.
2. Scott J Antonia, Augusto Villegas, Davey Daniel, et al. Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC. N Engl J Med. 2018 Dec 13;379(24):2342-2350. doi: 10.1056/NEJMoa1809697.
3. Jhanelle E Gray, Augusto Villegas , Davey Daniel, et al. Three-Year Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC-Update from PACIFIC. J Thorac Oncol. 2020 Feb;15(2):288-293. doi: 10.1016/j.jtho.2019.10.002.
4. Corinne Faivre-Finn, David Vicente, Takayasu Kurata, et al. Four-Year Survival With Durvalumab After Chemoradiotherapy in Stage III NSCLC-an Update From the PACIFIC Trial. J Thorac Oncol. 2021 May;16(5):860-867. doi: 10.1016/j.jtho.2020.12.015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PACIFIC#
95
#III#
80
#mAb#
67
#Oncol#
76
#THORAC#
83
#放化疗#
76
#III期#
66
JTO上有很多不错的好文章,谢谢梅斯及时上新
95
谢谢梅斯分享这么多精彩信息
88
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
79