Nat Commun:单细胞分析揭示移植瘤和原发性肉瘤的不同免疫状况并影响免疫疗法的效果
2020-12-22 xiaozeng MedSci原创
许多癌症患者通过接受放射性治疗(RT)来进行治疗或缓解症状。既往研究显示,免疫疗法并不能治愈大多数癌症患者。临床前研究显示,局部RT治疗可通过与免疫检查点抑制剂进行协同作用,以产生全身性抗肿瘤免疫反应
许多癌症患者通过接受放射性治疗(RT)来进行治疗或缓解症状。既往研究显示,免疫疗法并不能治愈大多数癌症患者。临床前研究显示,局部RT治疗可通过与免疫检查点抑制剂进行协同作用,以产生全身性抗肿瘤免疫反应。
然而,大多数临床前免疫疗法研究主要采用了移植瘤模型,在联合免疫检查点阻滞以及RT后,显示出较高的治愈率。然而该模型高估了患者的反应,也导致了许多临床试验中新发的结果令人失望。
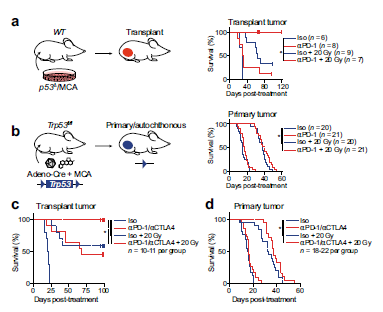
阻断PD-1联合放疗可治愈移植瘤但不能治愈原发性肉瘤
在该研究中,研究人员发现,通过阻断PD-1联合放疗可以治愈移植性肉瘤,然而该治疗策略在原发性肉瘤中治疗失败,这说明免疫编辑、新抗原表达降低以及肿瘤特异性免疫耐受的发生。
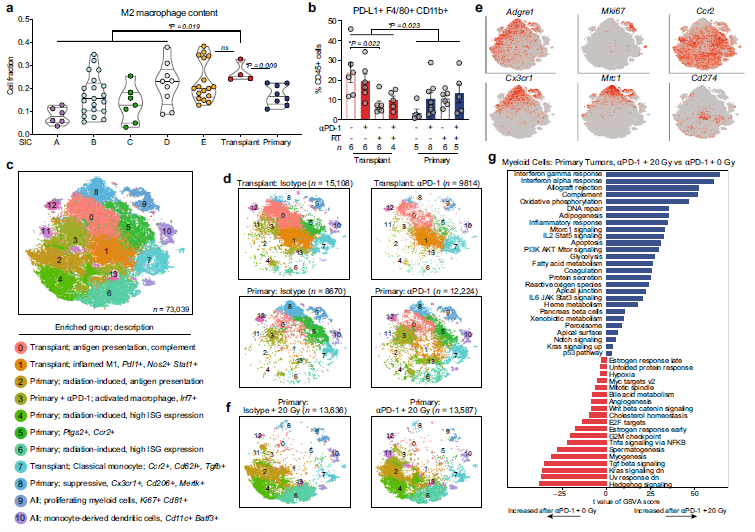
肿瘤和治疗促进了骨髓细胞的重塑
研究人员进一步的在移植瘤和原发性肿瘤中鉴定了肿瘤浸润相关的免疫细胞,并揭示了其免疫状况的显著性差异。尽管在这两种模型中放疗疗法都重塑了骨髓细胞,但只有移植瘤中富含激活的CD8+T细胞。小鼠模型显示,原发性鼠肉瘤的免疫微环境与大多数人源肉瘤相似,而移植肉瘤则与炎性程度最高的人源肉瘤相似。
总而言之,该研究结果在小鼠肉瘤中发现了与免疫系统共进化的独特的免疫微环境。该研究结果也揭示了与移植瘤状态相似的肉瘤表型患者能够更好的通过阻断PD-1和放疗联合治疗的方式改善预后。
原始出处:
Wisdom, A.J., Mowery, Y.M., Hong, C.S. et al. Single cell analysis reveals distinct immune landscapes in transplant and primary sarcomas that determine response or resistance to immunotherapy. Nat Commun 11, 6410 (17 December 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#原发性#
96
#移植瘤#
169
#COMMUN#
97
#原发性肉瘤#
96
#Nat#
105
加油
136
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
113
加油
154