Cancer Cell:科学家或可成功预测白血病的发生
2016-01-15 佚名 生物谷
最近,发表于国际杂志Cancer Cell上的一项研究论文中,来自麦克马斯特大学等处的研究人员通过研究成功鉴别出了致死性癌症的早期发病阶段,同时也成功预测了这种疾病在机体中的发病机制。 研究人员Mick Bhatia教授指出,我们发现了从健康到癌性的血液干细胞的过渡常常发生在有区别的过程中,这项研究中我们鉴别出了两个关键的步骤。文章中研究人员对骨髓增生异常综合征(MDS)成功地进行了指纹图谱分析
最近,发表于国际杂志Cancer Cell上的一项研究论文中,来自麦克马斯特大学等处的研究人员通过研究成功鉴别出了致死性癌症的早期发病阶段,同时也成功预测了这种疾病在机体中的发病机制。
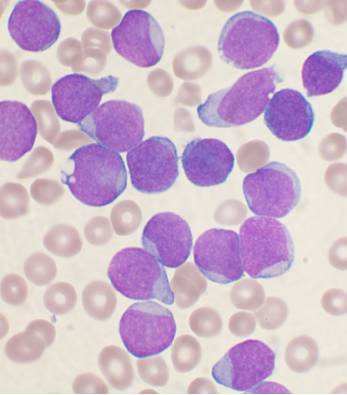
研究人员Mick Bhatia教授指出,我们发现了从健康到癌性的血液干细胞的过渡常常发生在有区别的过程中,这项研究中我们鉴别出了两个关键的步骤。文章中研究人员对骨髓增生异常综合征(MDS)成功地进行了指纹图谱分析,骨髓增生异常综合征是血细胞转化为急性髓性白血病(AML)的一个阶段,急性髓性白血病在白血病患者中大约占到了30%左右。本文研究为后期进行急性髓性白血病的准确和早期预测提供了一定可能。
急性髓性白血病是一种常见的成年人的白血病,每年大约有1300名加拿大人被预测会患上这种白血病;文章中研究者发现,当剔除名为GSK-3基因的一个链时(one version),另一部分就会被激活,但并不具有癌变性质,然而当该基因的第二部分(第二条链)也被剔除后就会导致急性髓性白血病的发生。
为了检测这一结果,研究人员同博洛尼亚大学的研究人员通过联合研究将初期的研究成果应用于对人类血液样本进行研究,这些血样收集自MDS患者,其中有些患者最终患上了急性髓性白血病;文章中研究人员进行了一项追溯研究,结果表明,对患者血样的基因表达分析可以帮助准确预测哪些患者会患上急性髓性白血病,而哪些患者不会患病。
最后研究人员说道,本文研究或可帮助他们鉴别哪些MDS患者会患上急性髓性白血病,然而下一步研究人员将进行更深入的研究来预测多种血液癌症,通过利用预测性基因的表达作为药物靶点来帮助抑制疾病的发生,当然这对于开发新型治疗多种白血病的药物也提供了很好的线索和依据。
原始出处:
Borhane Guezguez, Mohammed Almakadi,et al.GSK3 Deficiencies in Hematopoietic Stem Cells Initiate Pre-neoplastic State that Is Predictive of Clinical Outcomes of Human Acute Leukemia.Cancer Cell.Jan 11,2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#cancer cell#
75
#CEL#
62
#Cell#
71
人类的进步
153
血液病太折磨病人
140
一大进步
121