J Am Coll Cardiol :仅四分之一急性心肌梗死合并心源性休克患者实现了完全血运重建,残余SYNTAX评分与这类患者的死亡率独立相关
2021-01-31 心关注 心关注
在多支血管病变合并心肌梗死(MI)相关心源性休克(CS)患者中,使用多支血管PCI策略治疗的患者中只有1/4能够实现完全血运重建。残余SYNTAX评分与早期和晚期死亡率独立相关。
在多支血管病变合并心肌梗死(MI)相关心源性休克(cardiogenic shock,CS)患者中,使用多支血管PCI(multivessel percutaneous coronary intervention,MV-PCI)策略治疗的患者中只有1/4能够实现完全血运重建(complete revascularization,CR)。残余SYNTAX评分与早期和晚期死亡率独立相关。
患有多支冠状动脉疾病(CAD)合并急性心肌梗死(MI)相关心源性休克的患者很少实现完全血运重建。作为一个可量化的、重复性好的术前解剖评估系统,SYNTAX评分自2005年第一次提出以来,显示了良好的预后评估效果,并被欧美指南推荐应用于临床。近日,发表在JACC上的一项研究评估了CS患者残余SYNTAX评分的预测价值。结果显示,残余SYNTAX评分与早期和晚期死亡率独立相关。
这些发现是通过对CULPRIT-SHOCK(CS患者单纯罪犯病变PCI[CLO-PCI] vs. MV-PCI)试验的亚分析获得的。该分析旨在通过使用与MI相关的心源性休克患者的残余SYNTAX评分,来评估PCI术后残余冠状动脉狭窄的程度、严重程度和预后价值,以及评价残余SYNTAX评分对早期和晚期预后的影响。
2017 TCT会议期间公布的CULPRIT-SHOCK试验比较了MV-PCI策略与CLO-PCI策略在以MI相关CS为表现的多血管CAD患者中的作用。法国巴黎索邦大学心脏病学研究所Olivier Barthélémy教授等人注意到,研究结果表明,与多支CAD合并MI相关CS患者同期MV-PCI策略相比,择期血运重建的CLO-PCI策略显着降低了30天死亡率或肾替代疗法的发生率(主要为30天内死亡率的降低)。
这些结果导致了目前欧洲心脏病学会(ESC)关于心肌血运重建的指南,不再推荐这种情况下直接PCI期间行常规非梗死相关动脉PCI(Ⅲ级,证据级别:B)。而这与血流动力学稳定的MI患者相反,后者在PCI或冠状动脉旁路移植术(CABG)后立即或早期完全血运重建被证明与更好的心血管结局相关。
在本研究中,Barthélémy等人对2013年4月-2017年4月在83个欧洲中心进行的CULPRIT-SHOCK试验中涉及的706名患者的冠状动脉造影进行了分析。由经验丰富的血管造影读片者通过视觉评估SYNTAX评分,其对临床和手术数据不知情。使用在线SYNTAX评分工具对直径≥1.5 mm、血管狭窄≥50%的病变进行评分。两个读片者独立阅片,评估基线和残余SYNTAX评分,并将数据输入专用的计算机数据库。
如果在首次住院期间进行了择期非罪犯病变血运重建,则基线SYNTAX评分评估是预先指定和前瞻性计算的,而残余SYNTAX评分是在CLO-PCI组首次PCI或计划内PCI血管造影的最后一帧上计算的。研究结局包括30天死亡率或肾脏替代治疗(CULPRIT-SHOCK试验的主要终点)以及30天死亡率和一年死亡率。
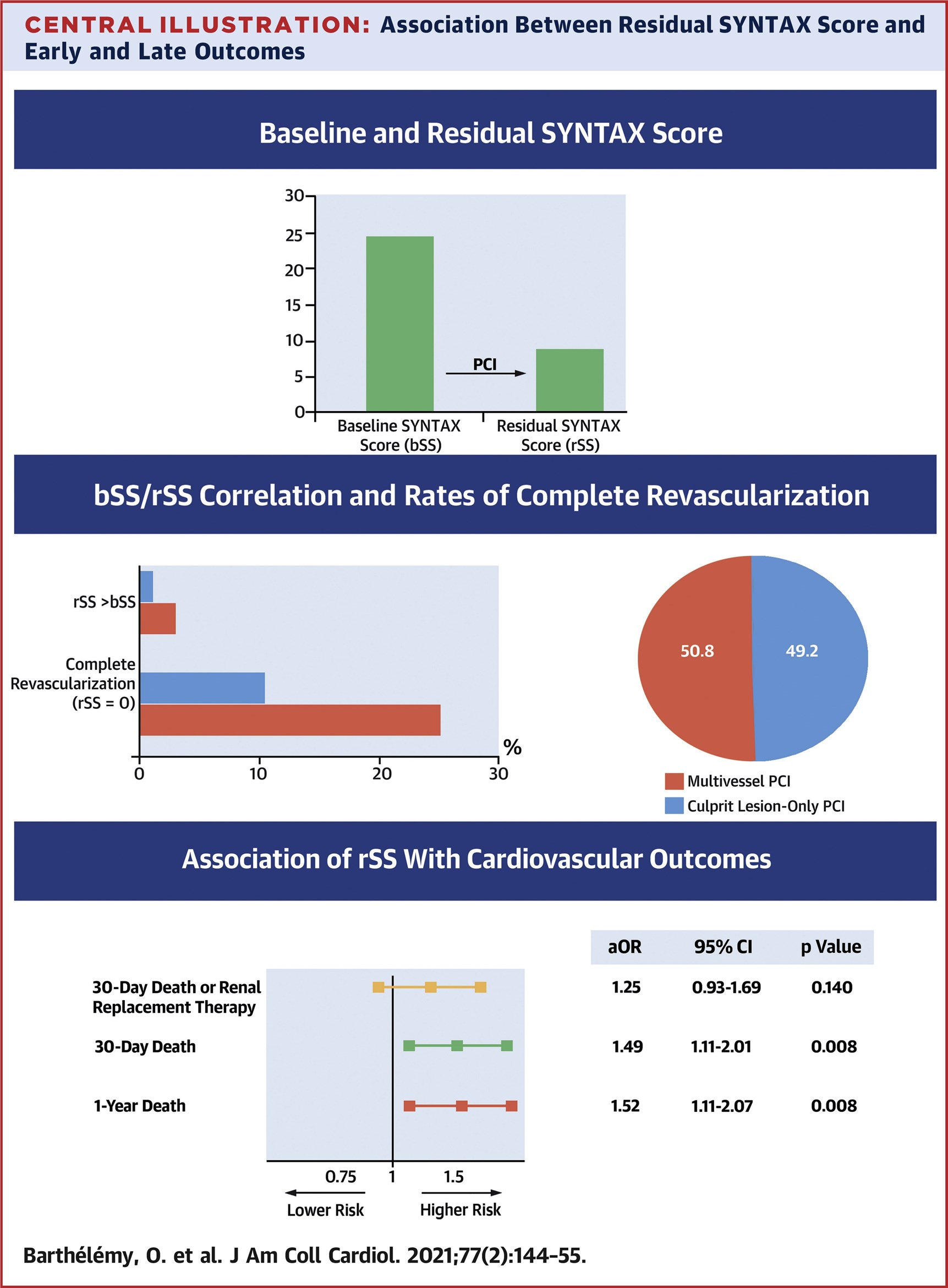
在CULPRIT-SHOCK试验随机抽取的706名患者中,587名(85.6%)被纳入了亚研究。在这些患者中,PCI前基线SYNTAX评分中位数为24.5(四分位间距[IQR] 17-32)。有298名患者(50.8%)进行了同期MV-PCI,而在该研究CLO-PCI组随机分组的289名患者(49.2%)中,48名患者(16.6%)在随机分组后9天内(IQR 4-18)进行了择期PCI。在整个研究组中,残余SYNTAX评分中位数为9(IQR 3-17),102名患者(17.4%)实现了完全血运重建。采用MV-PCI和CLO-PCI治疗的患者中,分别有75例(25.2%;95CI 20.3%-30.5%)和27例(9.3%;95%CI 6.2%-13.3%)实现完全血运重建。多次调整后,残余SYNTAX评分与30天死亡率(每10个单位的校正比值比:1.49;95%CI 1.11-2.01)和1年死亡率(每10个单位的校正比值比:1.52;95%CI 1.11-2.07)独立相关。作者进一步指出,在整个研究组中,随着残余SYNTAX评分的增加,结局发生率逐步增加,就像在每个随机分组中一样。
研究人员表示,该研究是第一个在大样本中评估与AMI相关的CS中残余SYNTAX评分的预后价值的研究,结果发现尽管使用了MV-PCI策略,但完全血运重建仅在四分之一的患者中实现。此外,研究人员还注意到残余SYNTAX评分与早期和晚期死亡率相关,与所有临床特征和基线SYNTAX评分无关。
如该研究所示,作为心血管结局独立预测因子的高残余SYNTAX评分与CULPRIT-SHOCK试验结果之间存在明显差异,后者显示CLO-PCI与MV-PCI策略相比具有优势。研究人员推测CS患者的这些差异,可能与以下因素有关:1)基线时更严重的CAD模式;2)PCI后较难实现的完全血运重建;3)有害的补充PCI风险较高。
在CLO-PCI和MV-PCI组中,1~3%患者的残余SYNTAX评分高于基线SYNTAX评分,其直接PCI导致冠状动脉解剖恶化,这种情况从未在血流动力学稳定的患者中描述过。这一发现考虑是通过残余SYNTAX评分,在成功的PCI术后发现罪犯冠状动脉全闭塞的下游隐藏的狭窄,而不是基线SYNTAX评分评估。然而,非罪犯病变的处理似乎是预后的关键决定因素。在急性情况下,高估非罪犯病变的严重程度,从而对非血流限制性狭窄进行PCI,甚至可能造成伤害,这是一个明显的风险。
研究人员指出,更完全的血运重建和更安全的血运重建可能是这一领域未来临床研究的目标,机械循环支持装置可能会对此提供答案。这些设备是否应该用于急性心肌挽救,非急性择期血运重建,或两者兼有,以实现更完全的血运重建仍然是一个争论的问题。
原始出处:
Olivier Barthélémy, Stéphanie Rouanet, Delphine Brugier,et al.Predictive Value of the Residual SYNTAX Score in Patients With Cardiogenic Shock.J Am Coll Cardiol. 2021 Jan 19;77(2):144-155. doi: 10.1016/j.jacc.2020.11.025.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SYNTAX评分#
61
#Coll#
56
#Cardiol#
66
#心源性休克#
72
#心源性#
0
#完全血运重建#
68
学习了
114