Curr Bio:由打哈欠引出的神经疾病治疗新思路
2017-09-04 佚名 生物探索
看见别人打哈欠,自己是不是也会不由自主地打哈欠呢?然后你会好奇:打哈欠会传染吗?为什么?最近,来自于诺丁汉大学的科学家们发现,这种传染性行为源于大脑控制运动机能的特定区域——初级运动皮质层的“原始反射”。这种本能的冲动程度受皮质兴奋性控制。
看见别人打哈欠,自己是不是也会不由自主地打哈欠呢?然后你会好奇:打哈欠会传染吗?为什么?最近,来自于诺丁汉大学的科学家们发现,这种传染性行为源于大脑控制运动机能的特定区域——初级运动皮质层的“原始反射”。这种本能的冲动程度受皮质兴奋性控制。
他们的研究以“A neural basis for contagious yawning”为题,于8月31日发表在Cell子刊《Current Biology》。这是对神经类疾病潜在生物学特征的另一种解析,有望为疾病的治疗提供新的方法。
心理学学院的认知神经科学教授Stephen Jackson和团队发现,当看到周围人打哈欠时,我们抵抗自己跟着打哈欠的能力相对有限。而且,我们抵抗的决心越大,我们打哈欠的欲望也会增加。无论我们多么努力地抑制打哈欠,都不会影响打哈欠的欲望。更重要的是,研究人员发现,打哈欠传染的冲动因人而异!
“打哈欠传染”并不局限于人类
当我们发现其他人在打哈欠时,自己常常也会不由自主地打哈欠——这是Echophenomena(模仿症)的一种常见表现。除此之外,Echophenomena还包括模仿他人的语言(echolalia)和动作(echopraxia)。
这种模仿行为不仅仅局限于人类之间,狗狗和猩猩同样也有这样的倾向。在临床上,Echophenomena还与皮质兴奋增加、生理抑制减少相关的疾病有关,例如痴呆、自闭症等疾病。
Stephen Jackson教授认为,这一发现有助于深入了解运动应激性和模仿症(Echophenomena)之间的关联,从而为癫痫、痴呆、自闭症等疾病提供新的线索。
打哈欠传染为什么因人而异?
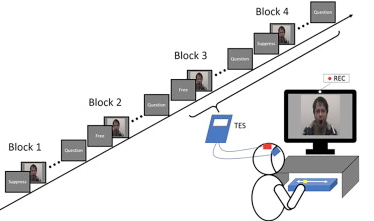
试验模拟图(图片来源:文献)
为了弄清楚运动兴奋性与打哈欠传染之间的关联,研究团队招募36名成年人,采用经颅磁刺激技术(transcranial magnetic stimulation,TMS)进行试验。这些志愿者被随机分组,通过观看别人打哈欠的视频片段被要求控制不打哈欠/允许打哈欠。这一过程全程被记录,包括他们每次打哈欠的次数。经颅磁刺激技术被用于量化每个参与者运动皮质兴奋性以及生理抑制的程度,从而预测所有志愿者传染性打哈欠的冲动强度。
结果表明,每个人皮质层的“兴奋性”影响着打哈欠的冲动。每个人大脑皮质兴奋性和主要运动神经系统的生理抑制决定其模仿打哈欠的冲动程度,从而导致个体差异。当抑制冲动时,反而会增强它。“通过电刺激,我们能够增加兴奋性,从而增加传染性打哈欠的冲动。如果我们降低兴奋度,或许我们可以减少冲动。” 心理健康研究所的认知神经心理学教授Georgina Jackson解释道。
Stephen Jackson教授表示:“如果我们知道皮质兴奋性导致神经紊乱的机理,我们就有机会逆转它。我们正在寻找潜在的非药物、个性化治疗方法,例如利用TMS技术调控大脑神经网络中的不平衡。”
原始出处:
Beverley J. Brown, Soyoung Kim, Hannah Saunders, et,al. A Neural Basis for Contagious Yawning. Current BiologyAugust 31, 2017
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Bio#
88
#疾病治疗#
70
#新思路#
74
#神经疾病#
92