BMJ:低剂量CT筛查对肺癌患者疾病分期及生存期的影响
2022-04-02 zhangfan MedSci原创
低剂量CT肺癌筛查方案大幅提高了I期NSCLC患者比例,延长患者生存期

尽管晚期肺癌治疗进展显著提高了患者生存率,但肺癌早期筛查仍然是降低肺癌死亡率的重要手段,研究已证实了低剂量CT对肺癌早期筛查的效果。近日研究人员评估了低剂量CT筛查方案在2014年实施后对美国肺癌分期及生存期的影响。
研究人员收集了美国国家癌症数据库和主要流行病学数据库数据,参与者为2010-18年间确诊的非小细胞肺癌患者,年龄45-80岁。研究的主要终点为45-54岁(非筛查人群)和55-80岁(筛查人群)中I期NSCLC患者比例的变化、早期疾病以及筛查前后死亡风险变化。
研究发现,对于55-80岁人群,2010-13年间,I期NSCLC患者比例变化不显著(27.8%-29.4%),2014-18年间,I期NSCLC患者比例每年增加3.9%,从30.2%提高到35.5%。研究发现,首次诊断为低分期肺癌的患者比例,2014-18年间,每年增加约6.2%,高于2010-13年的数据。2010-13年间,55-80岁人群的肺癌生存期无显著变化(15.8-18.1个月),但2014-18年间,生存期每年增加11.9%,从19.7个月增加到28.2个月。相比于2014年前,2014年后患者死亡率显著下降。到2018年,在非西班牙裔白人、高收入以及良好教育人群中,I期NSCLC患者占初次肺癌诊断的绝大多数,而非白人、低收入以及低学历人群中,IV期占初次肺癌诊断的绝大多数。肺癌初次诊断时早期疾病占比提高,大大减少了死亡人数,从2014-18年,累计减少10100人死亡。
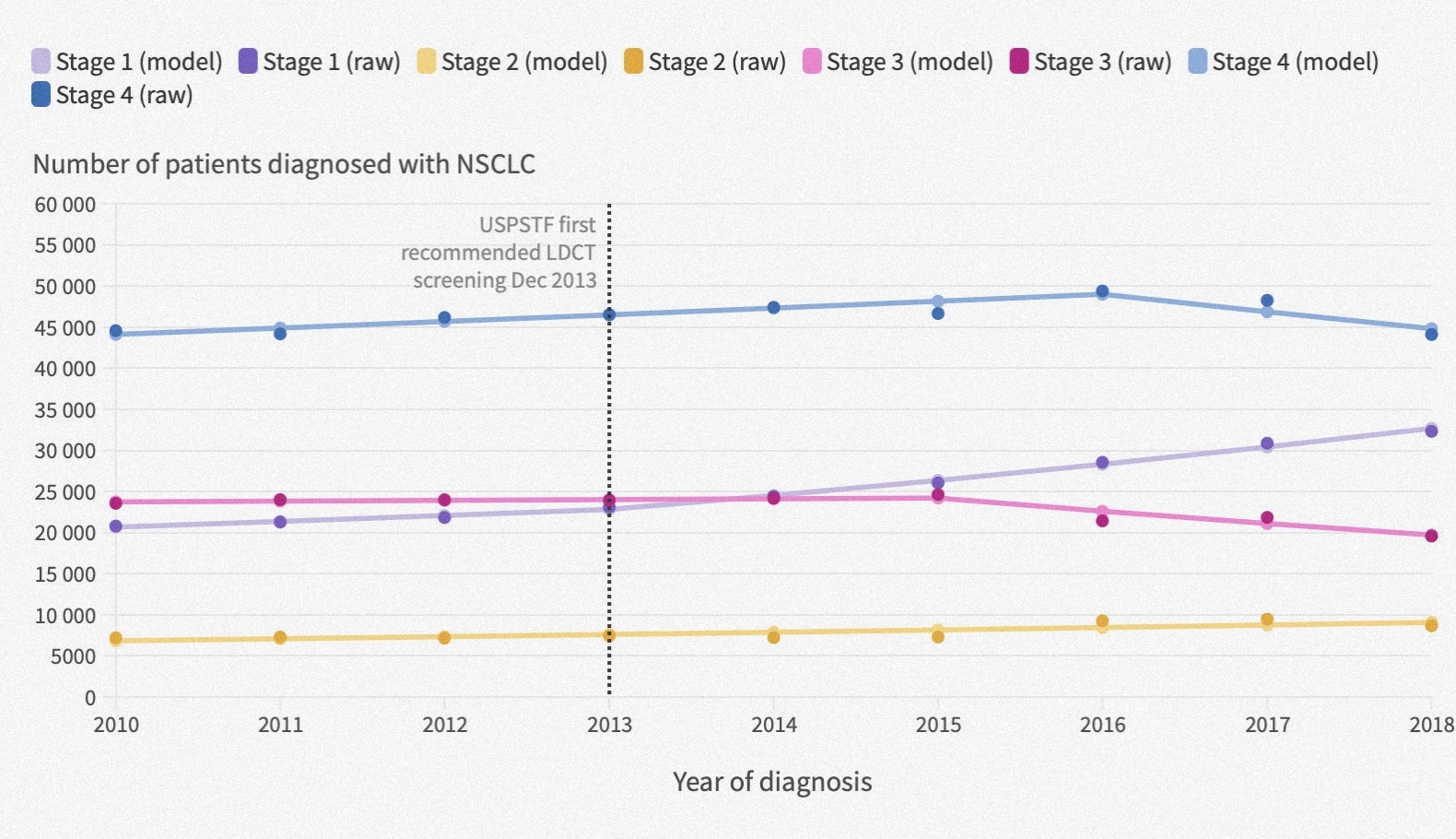
CT筛查方案大大提高了早期疾病患者比例
研究认为,低剂量CT肺癌筛查方案大幅提高了I期NSCLC患者比例,延长患者生存期。
原始出处:
lexandra L Potter et al. Association of computed tomography screening with lung cancer stage shift and survival in the United States: quasi-experimental study. BMJ,30 March,2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CT筛查#
101
#BMJ#
61
#肺癌患者#
67
#生存期#
69
#低剂量CT#
81
#低剂量#
54