Front Oncol:原发肿瘤大小对结直肠癌(CRC)生存的预测和预后影响
2021-12-11 yd2015 MedSci原创
研究表明,今后需要进一步的研究来阐明肿瘤大小在预后分期模型中的作用,以及如何将其纳入治疗决策。
病理分期对于结直肠癌(CRC)患者的治疗至关重要。但是结直肠癌(CRC)患者的T分期根据肿瘤浸润的深度,并不考虑肿瘤大小。因此,CRC患者的肿瘤大小对于临床预后的影响尚不明确。因此,来自美国的学者开展了一项基于人群的大型回顾性研究,评估了原发肿瘤大小对所有分期结直肠癌患者的预测和预后影响。相关结果发表在Frontiers in Oncology杂志上。
研究者利用国家癌症数据库(NCDB),对2010年至2015年接受原发肿瘤切除术的CRC患者进行了分析。使用单因素和多因素分析来确定预测和预后因素,Kaplan-Meier分析和Cox比例风险模型来确定肿瘤大小和生存之间的关系。
研究纳入60,999例患者,中位诊断年龄为62.7岁(SD+/-14)。50.9%为男性。82.7%为结肠癌。AJCC分期为:I -20.1%;2 - 32.1%;III - 34.7%和IV - 13.1%。原发性肿瘤大小以小于2-5cm的居多(50.8%),其次为5-10cm(32.6%)、<2cm(13.1%)和>10cm(3.4%)。多数肿瘤为中分化(68.7%),82%为微卫星稳定型(MSS)。与较小的原发肿瘤(小于2cm)相比,大于10cm的原发肿瘤更有可能出现晚期疾病(IV期:19% vs. 5%;p<0.001),具有更多的微卫星不稳定性(MSI- H: 32.9% vs. 12.7%;P<0.001),且直肠起源的更少(9.6% vs. 25.7%;p<0.001)。
I期患者中,2-5cm (50.2%)最常见,其次<2cm(37.8%),>10cm(<1%)。II期患者中,肿瘤大小分布在2-5cm(49%)和5-10cm(40.7%)之间。肿瘤大小为<2cm(5.5%)或>10cm(4.8%)的患者较少。III期患者中,肿瘤大小分布为<2cm(8.9%)、2-5cm(54%)、5-10cm(34.1%)和>10cm(3%)。IV期患者中,原发肿瘤大小分布为<2cm(5.2%)、2-5cm(47.8%)、5-10cm(42%)和>10cm(5.1%)。
与肿瘤大小<2cm的患者相比,肿瘤大小对整个研究人群的预后具有显著的影响,2-5cm (HR=1.20;1.13-1.28;P<0.001),5-10cm(HR=1.38;1.30-1.48;p<0.001)和>10cm (HR=1.55;1.41 - 1.71;P<0.001)患者预后更差。多因素分析,AJCC分期与OS显著相关(与I期相比,II-III期的HR分别为1.44, 2.21,和8.10)。

根据分期和肿瘤大小进行预后分析

根据肿瘤大小进行多因素相关分析
在II期患者中,与肿瘤大小<2cm患者相比, 2-5cm(HR=0.99;0.86 - 1.15;p=0.942), 5-10cm (HR =1.04;0.90-1.21;p=0.583)或>10cm (HR 1.17;0.96-1.44;p = 0.123)患者的预后没有统计学差异。
在III期患者中,与肿瘤大小<2cm患者相比, 2- 5cm (HR=1.33;1.19-1.49;p<0.001), 5-10cm (HR 1.51;1.34 - 1.70;p<0.001)和>10cm (HR=1.95;1.65-2.31;P<0.001)患者的预后更差。
IV期结肠癌患者的中位总生存期按肿瘤大小进行分层:肿瘤大小<2cm患者的中位总生存期为34.3个月;2-5cm患者为30.3个月;5-10cm患者为23.7个月,>10cm为21.4个月。而相应的IV期直肠癌患者中位生存期分别为47.6, 40.7, 33.4 和34.1个月。
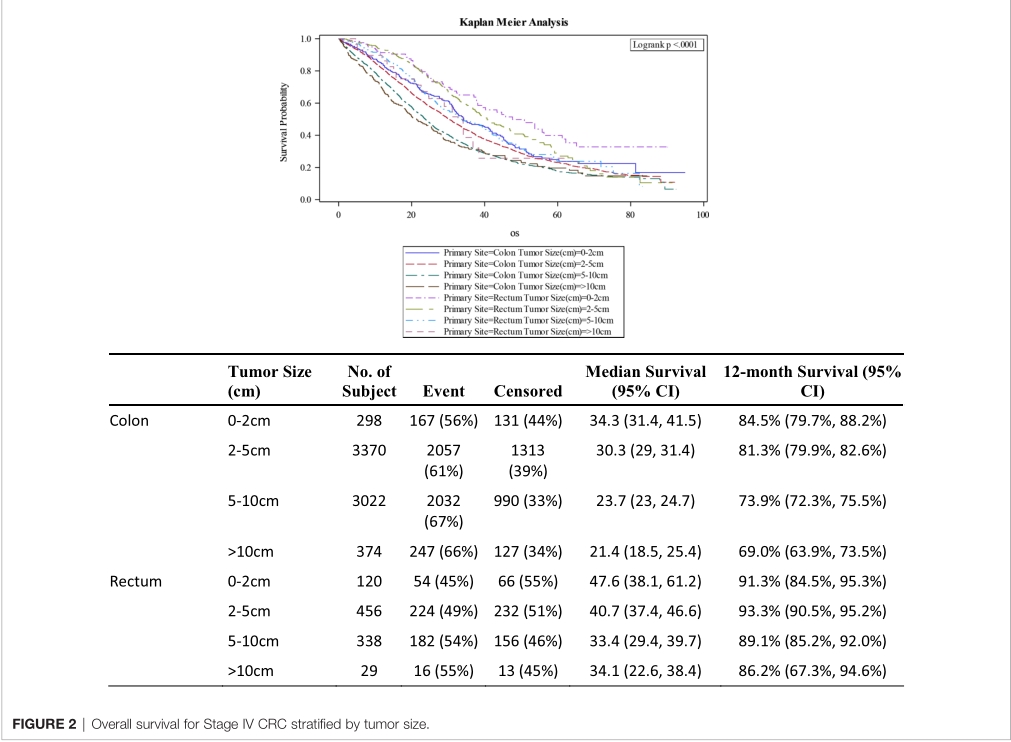
IV期患者根据肿瘤大小预后分析
将II期患者分为接受了辅助化疗的患者(n=6564)和未接受辅助化疗的患者(n= 13001),并与III期接受了辅助化疗的患者(n=19,155)和未接受辅助化疗的患者(n=2.007)进行比较。在确定辅助治疗时没有考虑肿瘤大小,并且在4个肿瘤大小类别中使用的辅助治疗是均匀分布的:<2cm, 2-5cm, 5-10cm和>10cm。II期未接受辅助化疗的患者预后跟III期接收辅助化疗患者相当(HR=1.09; 0.97-1.523;p=0.148)。而II期接收辅助化疗的患者较两组的预后都有改善(HR=0.76; 0.67-0.86; p<0.001)。在非转移性疾病亚组中,未接受辅助化疗的III期患者预后最差(HR=2.66;2.48-2.86;p<0.001)。
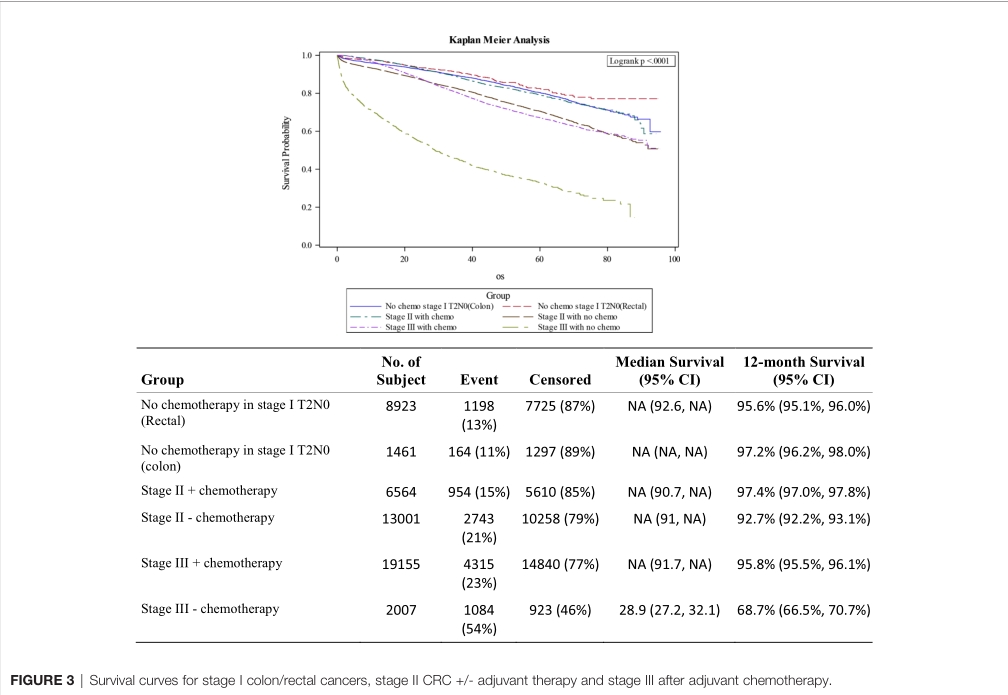
有无辅助化疗对预后影响
综上,研究表明,今后需要进一步的研究来阐明肿瘤大小在预后分期模型中的作用,以及如何将其纳入治疗决策。
原始出处:
Alese OB, Zhou W, Jiang R, Zakka K, Huang Z, Okoli C, Shaib WL, Akce M, Diab M, Wu C and El-Rayes BF (2021) Predictive and Prognostic Effects of Primary Tumor Size on Colorectal Cancer Survival. Front. Oncol. 11:728076. doi: 10.3389/fonc.2021.728076
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#原发肿瘤#
84
#CRC#
102
#Oncol#
80
学习了
91
#结直肠#
67
收益挺大
91
这个观点很有意思
106