JACC:房颤的发生率与心血管事件、心力衰竭、死亡相关
2015-08-25 MedSci MedSci原创
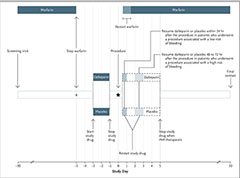
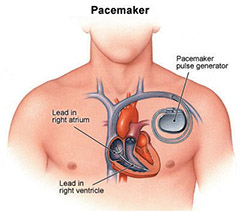
在治疗房颤(AF)相关的疾病方面已经做出了重要改善,如高血压,心肌梗塞和心脏衰竭。发病率和风险因素可能会随着人们年龄和生活方式的改变而改变。目前,房颤的风险只能部分地解释,可能是因为旧的队列和当代人群之间的差异。本研究探讨了荷兰的现代人群房颤的发病率,相关的合并症以及AF与心血管结果联系。PREVEND研究(肾和血管终末期疾病的预防)中8,265名参与者的AF事件是由医院和研究的心电图确定的,该研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
0
#发生率#
0
#血管事件#
70
#ACC#
68