Cancer cell:那些促进肿瘤生长,还吃PD-1抗体的巨噬细胞,科学家终于找到消灭你的好办法了
2017-12-05 姬亚茹、王新凯 奇点网
近年来的研究就发现,在肿瘤中总重量的50%竟然是巨噬细胞。这些肿瘤相关巨噬细胞(Tumor-associated macrophage, TAM)不仅会阻止T细胞攻击肿瘤细胞,而且还会分泌生长因子滋养肿瘤细胞,促进肿瘤血管的生成,导致肿瘤细胞转移扩散。
巨噬细胞真是个神奇又可怕的存在。尤其是和癌细胞走得近的巨噬细胞。
近年来的研究就发现,在肿瘤中总重量的50%竟然是巨噬细胞。这些肿瘤相关巨噬细胞(Tumor-associated macrophage, TAM)不仅会阻止T细胞攻击肿瘤细胞,而且还会分泌生长因子滋养肿瘤细胞,促进肿瘤血管的生成,导致肿瘤细胞转移扩散。
“失足”的巨噬细胞究竟会使多大的坏,大家可能都想象不出来。今年5月份,奇点君就写了由于巨噬细胞“捣乱”导致肿瘤免疫治疗对部分患者无效的报道。
更奇怪的是,科学家在“清理门户”的时候发现,清除这些叛变的肿瘤相关巨噬细胞并没有啥用,肿瘤细胞该继续生长还继续生长,免疫系统该被抑制还是被抑制。科学家们也是相当困惑,这背后究竟还有什么不为人知的原因。
就在本月,来自斯坦福大学的研究人员终于发现了一味地消除肿瘤相关巨噬细胞并未显示出抗肿瘤效果的原因,原来在使用CSF-1R抑制剂“清理”肿瘤相关巨噬细胞的同时,竟然会意外地招募一类有着强大免疫抑制活性的细胞积累。这些抑制性细胞的存在,对免疫系统的攻击力有着强大的抑制作用。真是“送走了小鬼,又来了阎王”。
更为重要的是,研究人员创造性地联合使用另一种抑制剂,在使用CSF1R抑制剂清除巨噬细胞的同时,避免抑制性细胞的积累和肿瘤免疫抗性的产生。研究表明,同时使用这两种抑制剂,不仅能够有效清除这些叛变的巨噬细胞,而且能够显着降低肿瘤的生长,并且在配合PD-1抑制剂组合治疗时,产生了更加强烈的抗肿瘤效果。相关研究成果发表在近期的《Cancer Cell》中。
肿瘤相关巨噬细胞
其实很久以前科学家们就注意到了巨噬细胞与肿瘤发生发展的相关性,肿瘤相关巨噬细胞作为炎症与肿瘤之间重要的调节者,不仅抑制了免疫细胞的“抗癌”功能,而且还促进了肿瘤的血管生成、增殖、存活和转移,发挥着不可忽视的强大致癌、助癌作用。
而在这其中,不得不提CSF1R蛋白,因为就是它,介导了巨噬细胞在肿瘤组织中的存活和功能。因此,一开始科学家们就将靶向CSF1R消除巨噬细胞作为一种治疗策略。
巨噬细胞究竟有什么神奇的地方,清除了叛贼都还消除不了其影响,这到底是怎么回事呢?
为了一探究竟,在这项研究中,研究人员在黑色素瘤、肺癌、淋巴瘤、结肠癌和乳腺癌等小鼠模型中,给予使用能够清除肿瘤相关巨噬细胞的药物即CSF-1R抑制剂,结果发现在大多数肿瘤模型中,都未表现出肿瘤进展的延缓。
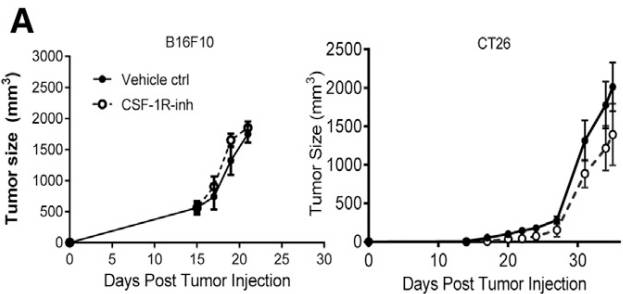
与对照组相比,注射药物后未能抑制小鼠模型的肿瘤生长
(Vehicle ctrl:对照组;CSF-1R-inh:消除肿瘤相关巨噬细胞药物)
经过进一步分析,研究人员惊讶地发现,虽然治疗后小鼠肿瘤组织中巨噬细胞数量出现了减少,但是却意外招募了大量多核型髓源抑制性细胞(PMN-MDSC)的积累。
免疫抑制是肿瘤患者治疗效果差、预后不理想的重要原因之一,而髓源抑制性细胞(MDSC)的存在,就会抑制免疫系统的攻击力,是肿瘤对于化疗、靶向疗法和免疫疗法等产生抗性的一个重要因素。目前已报道有多种病理类型的肿瘤患者体内可以检测到MDSCs,如肾癌、肺癌、黑色素瘤、肝癌、前列腺癌等。多核型髓源抑制性细胞(PMN-MDSC)就是其中最主要的一类。
研究人员通过查阅文献也发现,癌症患者血液中抑制性细胞的积累,的确与癌患者预后较差有关。
可是清除肿瘤相关巨噬细胞,怎么就意外地招募了大量的PMN-MDSC呢?
研究人员首先对比了使用CSF1R抑制剂的肺癌小鼠,并分析了肿瘤细胞裂解物中各种趋化因子的表达。结果发现与对照组相比,使用CSF1R抑制剂后会使肿瘤相关的成纤维细胞产生趋化因子(CXCL1)的数量显着增加,而这种趋化因子对招募免疫抑制细胞(PMN-MDSC)到肿瘤部位具有重要的作用。
原来不是巨噬细胞的问题,问题而是出在CSF1R抑制剂身上。既然知道了是CSF1R抑制剂的“错”,那CSF1R抑制剂究竟错在了哪里呢?是怎么错的呢?
研究人员发现,介导巨噬细胞功能和存活的CSF1的存在,是能够减少CXCL1趋化因子,从而避免免疫抑制细胞(PMN-MDSC)聚集的。但是,当使用CSF1R受体抑制剂时,就意外地消除了这种抑制,导致了CXCL1趋化因子的增加,从而引起免疫抑制细胞(PMN-MDSC)在肿瘤部位大量积累。
事已至此,可以说通过“清理门户”来斩掉癌症左膀右臂的策略遇到了“BUG”,毕竟这副作用还不如不“清理门户”呢。
但如果辩证地看,谜团的揭开也提供了一个创新的思路,那就是在使用CSF-1R抑制剂的同时,再想办法抑制CXCL1的数量,做到即清除肿瘤相关巨噬细胞,又不引起免疫抑制细胞的积累,从而达到抑制肿瘤的目的。
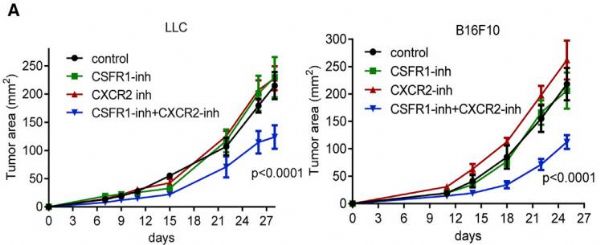
接下来的实验结果也表明了这个新思路的可行性以及良好的效果。研究人员在肺癌和黑色素瘤小鼠中模型中,同时加入消除肿瘤相关巨噬细胞的CSF1R抑制剂,和降低大多数趋化因子的药物选择性CXCR2抑制剂(CXCR2是CSF1R抑制剂上调大多数趋化因子的受体,其中包括CXCL1)
结果正如预期的一样,不仅显着抑制了肿瘤进展,而且减少了肿瘤相关巨噬细胞,也没有招募“抑制性细胞”的聚集。
使用CSFR1抑制剂和CXCR2抑制剂显着延缓了小鼠模型肿瘤进展

两种抑制剂联合使用能显着增强小鼠模型PD-1抗体抗肿瘤的效果
虽然目前针对肿瘤的疗法大多数都是通过恢复T细胞的功能来杀死癌细胞,如PD-1抗体和 CAR-T细胞疗法,但是却往往忽略了固有免疫细胞在其中的作用。在这项研究中,研究人员发现了在肿瘤浸润区的巨噬细胞,更多是发挥免疫抑制作用,尤其是发现了免疫抑制活性细胞(MDSC)被招募并积累的具体信号通路。
而且研究人员尝试将消除肿瘤相关巨噬细胞(CSF1R抑制剂),和降低趋化因子的药物(选择性CXCR2抑制剂)以及PD-1抗体联合使用,惊讶地发现抗肿瘤效果显着增强。与单独使用各种抑制剂的抗肿瘤作用相比,联合治疗能够显着降低肿瘤生长,并且能够显着增强PD-1抗体免疫治疗的效果,而这可能为肿瘤治疗创造新的机会。
原始出处:Kumar, V., Laxminarasimha Donthireddy, Douglas Marvel, et al., Cancer-Associated Fibroblasts Neutralize the Anti-tumor Effect of CSF1 Receptor Blockade by Inducing PMN-MDSC Infiltration of Tumors. Cancer Cell, 2017. 32(5): p. 654-668.e5.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#CEL#
84
#Cell#
67
#cancer cell#
69
不错不错
76
可以学习一下.
90
学习了.谢谢分享
84
#PD-1抗体#
70
最近关于巨噬细胞的确研究比较多
91
学习了新知识
69
谢谢分享.阅读
0