Clin Cancer Res:一线化疗加用大剂量维C是否可改善转移性结直肠癌患者预后
2022-08-09 MedSci原创 MedSci原创
化疗方案中加用维生素C时可显著延长携带RAS突变的转移性结直肠癌患者的无进展生存期
维生素C在癌症治疗中的应用可追溯到40多年前,两项回顾性研究报道,静脉应用大剂量维生素C治疗后晚期癌症患者的生存期得以延长。但是,在随后的前瞻性研究中,口服维生素C未得到相似的结果;可能是给药方式严重影响了维生素C的药代动力学。
该研究旨在比较大剂量维生素C联合FOLFOX±贝伐单抗与FOLFOX±贝伐单抗作为一线方案治疗转移性结直肠癌(mCRC)的疗效和安全性。
2017年至2019年期间,组织学明确诊断的、6-磷酸葡萄糖脱氢酶状态正常的、既往未针对转移病灶进行治疗的mCRC患者(n=442)被随机(1:1)分至对照组(FOLFOX±贝伐单抗)和实验组(大剂量维生素C[1.5g/kg·天]+FOLFOX±贝伐单抗)。主要终点是无进展生存期(PFS)。
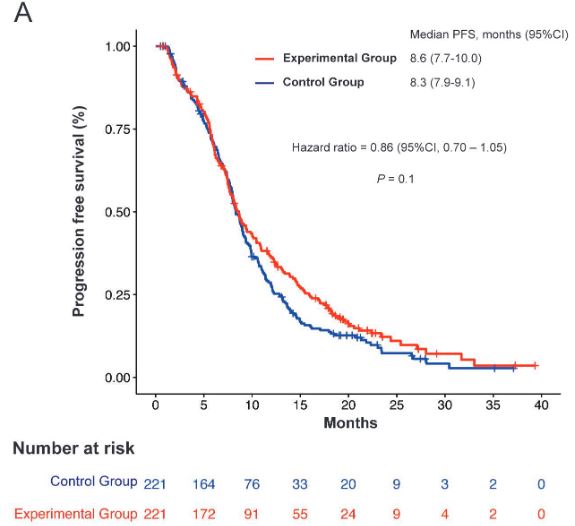
两组患者的无进展生存率
实验组的无进展生存期未明显优于对照组,中位PFS分别是8.6 vs 8.3个月(HR 0.86,p=0.1)。两组的客观缓解率(ORR)和总生存期(OS)均相差无几(ORR:44.3% vs 42.1%,p=0.9;中位OS:20.7 vs 19.7个月,p=0.7)。
携带RAS突变的患者的无进展生存率
实验组和对照组分别有33.5%和30.3%的受试患者经历了3级及以上的不良反应。在预定的亚组分析中,携带RAS突变的患者化疗方案中加用维生素C时可显著延长PFS(中位PFS:9.2 vs 7.8个月;HR 0.67,p=0.01)。
综上,大剂量维生素C联合化疗作为一项治疗方案未能相比化疗显著延长转移性结直肠癌患者的无进展生存期,但携带RAS突变的患者或可从加用维生素C治疗中获益。
原始出处:
Feng Wang, Ming-Ming He, Jian Xiao, et al. A randomized, open-label, multicenter, phase 3 study of high-dose vitamin C plus FOLFOX +/- bevacizumab versus FOLFOX +/- bevacizumab in unresectable untreated metastatic colorectal cancer. Clin Cancer Res 2022; https://doi.org/10.1158/1078-0432.CCR-22-0655.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#一线化疗#
60
#患者预后#
64
#转移性#
67
#结直肠#
71
#大剂量#
60