J Thorac Oncol:OAK研究再分析:NSCLC进展后继续阿替利珠单抗治疗仍可获益
2018-12-17 月下荷花 肿瘤资讯
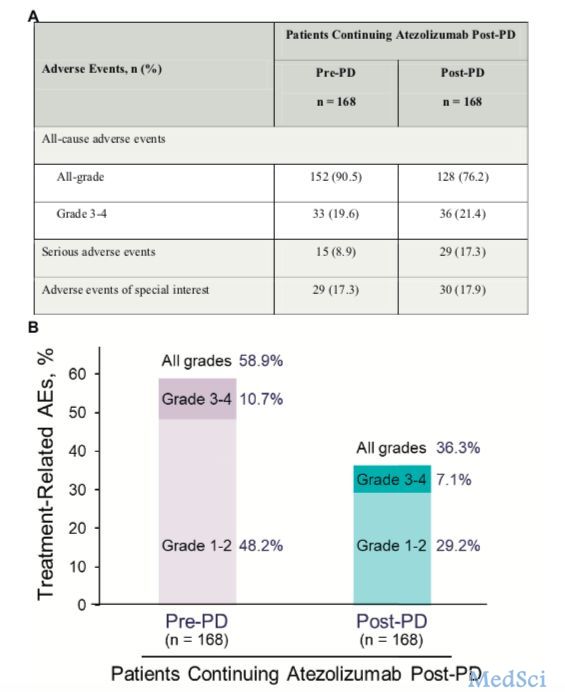
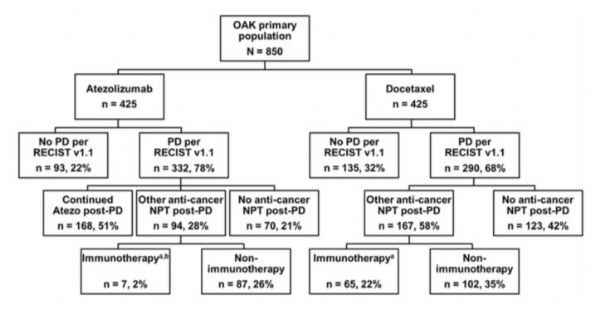
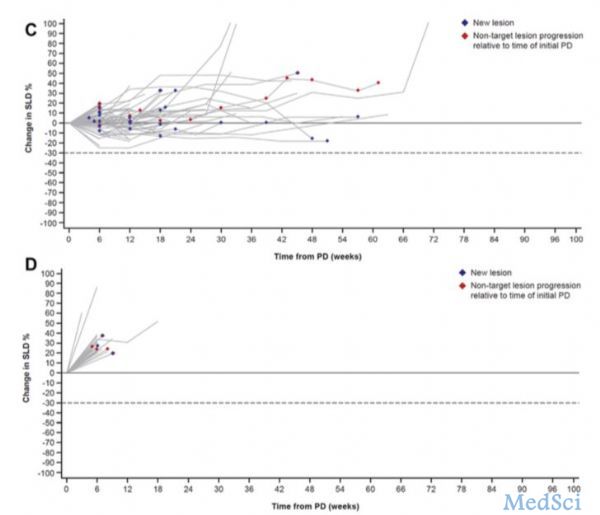
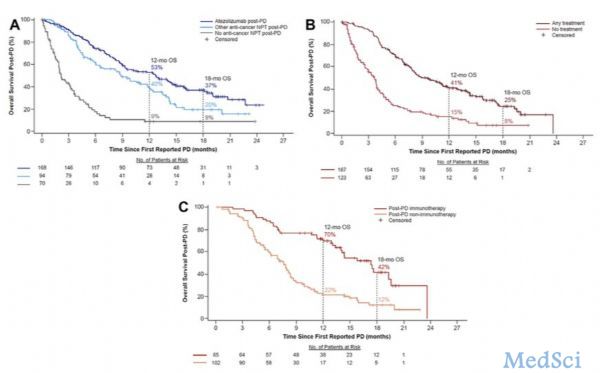
癌症免疫治疗可以改变肿瘤生物学,即便影像学进展时,治疗仍可能发挥作用。随机III期OAK研究中,进展期NSCLC接受阿替利珠单抗或多西他赛治疗,阿替利珠单抗治疗患者总生存(OS)获益,但客观反应率(ORR)或无进展生存(PFS)无改善。美国Gandara教授在J Thorac Oncol杂志上发文,对OAK研究进一步分析,结果表明进展后继续阿替利珠单抗治疗有良好的获益-风险比。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#THORAC#
56
#OAK研究#
43
#替利珠单抗#
126
#Oncol#
44
学习了
101