Cell Metab :四川大学曹中炜团队解析“循环微环境”调控衰老器官再生和纤维化
2020-12-31 BioArt Bio生物世界
组织的修复和再生对生物具有至关重要的作用。当组织在受到感染、机械损伤以及其他的刺激时,坏死的细胞或者入侵的微生物等会共同激活复杂的炎症反应。
组织的修复和再生对生物具有至关重要的作用。当组织在受到感染、机械损伤以及其他的刺激时,坏死的细胞或者入侵的微生物等会共同激活复杂的炎症反应。急性损伤时,伤口愈合反应通常会得到控制,炎症反应会迅速消退,并且正常组织结构也会恢复。但是,如果器官经历慢性损伤,伤口愈合反应往往是缓慢的或者处于失调状态,通常会导致病理性纤维化或瘢痕的形成,损害正常组织功能,并导致器官衰竭和死亡。
再生是在受损后重现原组织结构和功能而不会留下疤痕的能力,这种能力通常会随着年龄的增加逐渐减弱。纤维化可发生于各大主要器官。据估计,器官的纤维化与多达40%的疾病死亡相关。然而目前纤维化疾病的治疗手段和效果都很有限。因此研究如何促进纤维化器官的再生能力具有很强的临床价值。
成年人体内血管长度达到90,000km,血管腔内覆盖着10万亿到60万亿的血管内皮细胞,渗透到各个器官的各个细胞。长久以来血管都被认为是被动运输血液的导管。曹中炜和合作者丁楅森组以往一系列合作发现血管内皮细胞可以分泌angiocrine因子和血液系统细胞和蛋白质相互作用,从而形成“循环微环境”共同影响器官修复。
在这一过程中,循环微环境就像“土壤”一样,调控作为“种子”的实质细胞的功能。同时这一微环境具有很强的两面性,不同激活状态的微环境可以导致受损器官产生两种完全不同的结果,即:是发生再生还是变成纤维化(结疤)。因此解析循环微环境调控器官修复的具体分子细胞机制在再生医学中有理论意义。同时,因为循环系统具有易于干预(readily accessible)的特点,发掘器官修复中循环微环境中的具有独特功能的靶点有望开发相对高效的治疗手段。
2020年12月22日,四川大学华西二院/生物治疗国家重点实验室曹中炜课题组在Cell Metabolism 杂志在线发表题为:Aging Reprograms the Hematopoietic-Vascular Niche to Impede Regeneration and Promote Fibrosis 的研究论文。
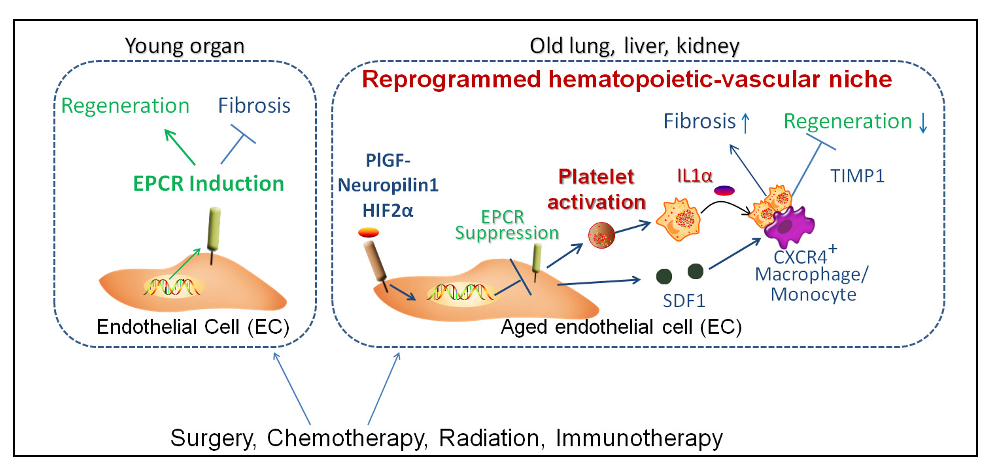
这一研究发现在衰老器官中血管内皮细胞和血小板,巨噬细胞一起形成了重编程的“循环微环境”,导致了衰老器官再生能力的抑制。同时,该研究还进一发现了调控这一微环境重编程过程的多重节点,即:靶向血管内皮细胞Neuropilin-1 (NRP1)、HIF2α,可以调控内皮细胞Endothelial Protein C Receptor (EPCR)的表达,进而影响血液中募集到的血小板interleukin-1 α (IL1α)以及巨噬细胞TIMP1的表达。特异性针对血管,血小板,和巨噬细胞的重编程节点分子可以使纤维化器官的循环微环境正常化,从而恢复受损器官的再生能力。
在衰老器官的循环微环境重编程中,内皮细胞的Endothelial Protein C Receptor (EPCR)通路抑制是再生到纤维化转变的一个重要节点。EPCR作为血管系统抑制炎症和血小板活化的关键分子,是由本文共同作者美国国家科学院院士,HHMI研究员Charles T. Esmon于1994年发现的。EPCR是一种内皮细胞特异性表达的位于细胞膜的跨膜糖蛋白,它是活化蛋白C(APC)介导的抗凝和细胞保护(抗炎、抗凋亡以及屏障稳定等)信号级联反应中的重要组成部分。其结构类似于主要组织相容复合物1/CDⅠ蛋白质家族,在调节炎症反应和血栓形成方面起重要作用。
血小板-巨噬细胞集落以及血管内皮细胞重编程导致衰老小鼠器官再生到纤维化的转变
作者通过肺切除模型比较对照鼠(2月龄或者3月龄)和老年鼠(20月龄)肺的再生和纤维化情况。通过染色发现,与年对照鼠相比,老年小鼠肺部血小板和巨噬细胞高表达,并紧密结合在血管细胞周围。这些数据表明,血液细胞参与了器官再生的调控,血小板和巨噬细胞之间异常的相互作用可能是衰老的肺中再生向纤维化转变的一个原因。
鉴于血管内皮细胞强大的旁分泌/自分泌功能,以及其与血小板-巨噬细胞集落的位置关系,作者分离了肺毛细血管内皮细胞(PCECs)进行转录组测序发现,Neuropilin-1 (NRP1)和HIF2α在老年小鼠中高表达,与之相反的是EPCR在老年小鼠PCECs中表达量降低。
为进一步研究血管内皮细胞与血液细胞之间的互相调控,作者构建了血管内皮细胞特异性敲除NRP1(Nrp1iDEC/iDEC)的基因鼠,与对照组相比,老年Nrp1iDEC/iDEC小鼠肺切后,HIF2α的表达量降低,EPCR表达水平上调,且Nrp1的敲除抑制了血小板-巨噬细胞集落的形成,纤维化程度降低,肺泡上皮细胞增殖明显增加。当抗体1560中和掉EPCR后,恢复了老年Nrp1iDEC/iDEC小鼠的血小板-巨噬细胞集落。PIGF作为NRP1的配体,在衰老的器官中表达上调。通过注射NRP1的不同配体,作者发现只有在注射PIGF时,可以抑制EPCR的表达。这说明内皮细胞中Nrp1可以调控EPCR的表达以及血液细胞:血小板-巨噬细胞集落的形成。
血小板产生IL1α激活促纤维化CXCR4+ TIMP1high巨噬细胞
因为血管中EPCR的表达为循环系统防止炎症和血小板活化的关键机制。作者进一步研究了衰老器官中血小板和巨噬细胞与EPCR被抑制的血管的相互作用,以及对器官修复的功能影响。血小板可以产生促炎性细胞因子,如白介素可与巨噬细胞相互作用。作者建了IL1α的血小板特异性缺失小鼠(Il1aDPlt/DPlt),在对小鼠进行EPCR中和抗体1560进行治疗后,发现Il1aDPlt/DPlt小鼠可阻断血小板-巨噬细胞集落的形成,并且能够降低TIMP1的表达。
通过血小板的移植模型,作者发现与移植Il1a+/+血小板的老年小鼠相比,移植Il1a-/-血小板的老年小鼠显示出TIMP1表达减少以及受试器官胶原沉积减少。这些数据提示抑制衰老ECs中的EPCR可以导致血小板IL1α的产生,而血小板IL1α参与了衰老器官中促纤维化血小板-巨噬细胞集落的形成以及TIMP1的表达。
靶向“循环微环境”的转化价值
针对EPCR的药物Activated Protein C(Xigris)于2001年11月21日被FDA批准为第一个用于治疗严重脓毒血症的生物药。此项研究有可能优化或开发针对EPCR的现有或者新一代的药物,从而发挥在纤维化器官的再生治疗方面的新作用。同时此项研究发现了EPCR在循环微环境中被抑制的上游调控机制。干预这一抑制机制有望上调EPCR,从而对EPCR上下游同时进行干预,进一步提升这一靶点的在纤维化疾病中的治疗效果。
为了验证所发现循环微环境调控作用的潜在治疗作用,作者团队在肺、肝、肾的再生和纤维化模型中都进行了验证。在肺,肝,和肾通过手术,化疗药物,放疗药物所导致的器官损伤中,选择性抑制血管内皮细胞中NRP1-HIF2α从而恢复EPCR的表达都起到了促进损伤器官组织结构和功能的恢复,防止了纤维化。尤其是研究结果证明了针对血管和血小板的节点分子的调控可以有效防止肺肿瘤免疫治疗引起的间质性肺炎 (Immunotherapy-induced pneumonitis)。在小鼠肺肿瘤的免疫治疗模型中,干预重编程的循环微环境不但降低了肺部的纤维化反应,而且延长了荷瘤小鼠的存活率。这一数据显示了循环微环境在多个损伤器官中的作为抗纤维化靶点的应用价值。
总之,该研究确定了靶向编辑血管内皮细胞中NRP1-HIF2α,血小板IL1α以及巨噬细胞TIMP1可以使原发性纤维化血液-血管微环境正常化,可恢复衰老器官的再生能力。
过去关于再生的研究大多局限于器官实质细胞本身,而此项研究发现了包括内皮细胞、血小板以及巨噬细胞在内的多细胞类型之间协同作用,形成一个多个分子参与在内的循环微环境。对这一调控机制的研究有望为纤维化器官的再生治疗研发靶点。
原始出处:
Yutian Chen, Qiang Pu, Yongyuan Ma,et al.Aging Reprograms the Hematopoietic-Vascular Niche to Impede Regeneration and Promote Fibrosis. Cell Metab . 2020 Dec 17;S1550-4131(20)30654-9. doi: 10.1016/j.cmet.2020.11.019.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#器官再生#
99
#Cell#
90
#解析#
82
#MET#
83
#四川大学#
94
#Meta#
63
#CEL#
64