Int Arch Occup Environ Health:在幼儿园工作能够增加听力相关症状的风险
2019-07-26 AlexYang MedSci原创
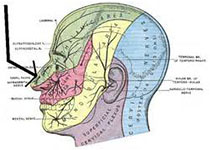
最近,有研究人员评估了是否在幼儿园工作能够增加听力相关症状的风险,以及是否年龄、职业噪音和压力工作条件能够影响上述风险。研究包括了4718名幼儿园教师和4122名随机挑选的对照。他们的年龄在24-65岁。研究人员通过调查问卷的方式对听力损失、耳鸣、语言感知困难和听觉疲劳等听力相关的症状进行了调查。研究发现,与对照相比,幼儿园教师的声音诱导的听觉疲劳(RR 2.4, 95%CI 2.2-2.5)和听
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ALT#
76
#听力#
74
#OCC#
89
#iron#
70
#Health#
72