Diabetic Med:以降低2型糖尿病和心血管疾病患者的HbA 1c水平为目标对并发症发生率进行建模
2018-03-25 MedSci MedSci原创
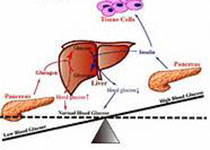
2型糖尿病的降糖干预显示微血管并发症减少,大血管并发症适度降低。然而,针对不同HbA 1c降低的程度可能降低风险尚不清楚。近日,国际杂志 《Diabetic Med》上在线发表一项关于以降低2型糖尿病和心血管疾病患者的HbA 1c水平为目标,对并发症发生率进行建模。 使用西格列汀(TECOS)心血管疾病参与者的评估心血管结局的参与者水平数据使用在2型糖尿病特异性模拟模型中,用于量化不同HbA
2型糖尿病的降糖干预显示微血管并发症减少,大血管并发症适度降低。然而,针对不同HbA 1c降低的程度可能降低风险尚不清楚。近日,国际杂志 《Diabetic Med》上在线发表一项关于以降低2型糖尿病和心血管疾病患者的HbA 1c水平为目标,对并发症发生率进行建模。 将西格列汀(TECOS)心血管疾病参与者的评估心血管结局数据应用在2型糖尿病特异性模拟模型中,用于量化不同HbA 1c递减对并发症发生率的可能影响。对于每个HbA 1c递减,得出每个结果的累计相对风险降低。 在2型糖尿病特定的模拟模型中采用了Sitagliptin (TECOS)参与者与已确定的心血管疾病患者的心血管预后评估的参与者水平数据来量化不同的HbA1c减量对并发症发生率的影响。通过在86,75,64,53 和42 mmol / mol(10%,9%,8%,7%和6%)的HbA 1c水平估计10年微血管和大血管的并发症速度,同时保持其他危险因素恒定在基准水平。利用每一个结果的累积相对风险降低推导HbA1c减量。 研究包括5717名参与者,72.0%为男性,74.2%欧洲白人,平均年龄为66.2(7.9)岁,收缩压1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病患者#
35
#发生率#
36
#BET#
35
#HbA#
27
#并发#
27
#DIA#
33
#Diabetic#
34
#血管疾病#
28
#Med#
36
学习了.长知识
63