Lancet oncol:采用人工智能检测上消化道癌症
2019-10-09 MedSci MedSci原创
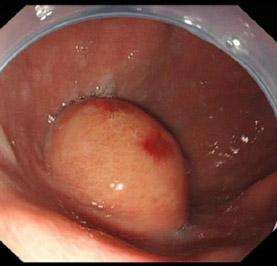
上消化道癌症(包括食道癌和胃癌)是世界范围内最常见的癌症。利用深度学习算法的人工智能平台在医学成像领域取得了显著进展,但在上消化道肿瘤领域的应用仍十分有限。现研究人员通过分析临床内镜的成像数据,开发和验证胃肠道人工智能诊断系统(GRAIDS),用于诊断上消化道肿瘤。本研究是在中国6家不同级别的医院进行的多中心、病例对照、诊断性的研究。纳入年满18岁的经病理学证实的上消化道恶性肿瘤患者,且要求具有标
本研究是在中国6家不同级别的医院进行的多中心、病例对照、诊断性的研究。纳入年满18岁的经病理学证实的上消化道恶性肿瘤患者,且要求具有标准白光的内镜图像。将来源于孙中山医院的图像按8:1:1分为开发GRAIDS的训练队列和内部验证队列,以及评估GRAIDS表现的外部验证队列,另5家医院的图像作为额外的外部验证队列。
84 424位个体的1036 496张内镜图像被用于开发和检验GRAIDS。在内部验证队列和前瞻性队列中,诊断上消化道癌症的准确性分别为0.955(95% CI 0.952-0.957)和0.927 (0.925–0.929);在5个外部验证队列中,准确性浮动在0.915(0.913-0.917)和0.977(0.977-0.978)之间。GRAIDS的诊断灵敏度与内镜专家的相近(0.942 vs 0.945,p=0.692),且优于内镜医生(0.858,p<0.0001)和内镜实习生(0.722,p<0.0001)。GRAIDS、内镜专家、内镜医生和内镜实习生的阳性预测值分别为0.814 (95% CI 0.788–0.838)、0.932 (0.913–0.948)、0.974 (0.960–0.984)和0.824 (0.795–0.850),阴性预测值分别是0.978 (95% CI 0.971–0.984)、0.980(0.974–0.985)、0.951(0.942–0.959)和0.904(0.893–0.916)。
GRAIDS在检测上消化道肿瘤时具有较高的诊断准确性,敏感性与内镜专家相近,优于非内窥镜专家。该系统有望帮助社区医院提高上消化道肿瘤诊断的有效性。
原始出处:
Huiyan Luo, et al.Real-time artificial intelligence for detection of upper gastrointestinal cancer by endoscopy: a multicentre, case-control, diagnostic study.The Lancet Oncology. October 04,2019. https://doi.org/10.1016/S1470-2045(19)30637-0
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Lancet#
80
#上消化道癌#
102
#Oncol#
72
#上消化道#
70
#消化道#
70
谢谢梅斯分享这么多精彩信息
84