N Engl J Med:TRACERx研究揭秘ctDNA系统进化:早期肺癌如何演变?
2017-08-06 佚名 肿瘤资讯
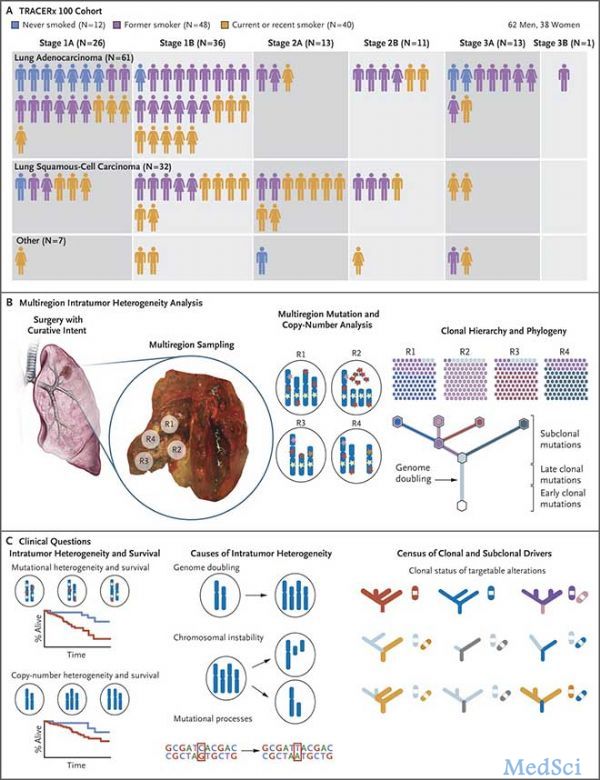
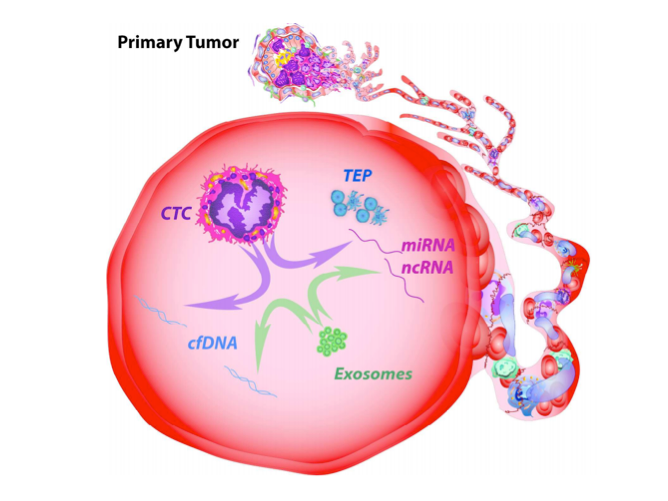
诸多研究表明肿瘤异质性是导致晚期肿瘤发生耐药、进展的始作俑者。迫于系统性治疗药物的选择压力,肿瘤细胞不断发生基因突变而分化为不同的亚克隆群体。那么,考虑到其形态和基因异质性均较高,早期肺癌的动态血ctDNA会有怎样的基因改变来驱动肿瘤进化以暗度陈仓呢?近期,英国Charles Swanton教授在Nature发表了TRACERx研究(TRAcking non-small cell lung Can
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









文献都不对,解读的根本不是原文链接里的文章
52
#演变#
81
#系统进化#
91
#Engl#
84
#早期肺癌#
85
#ACER#
83
#Eng#
74
#ACE#
99
#ACER#
82
#TRA#
104